Session Information
Date: Saturday, November 16, 2024
Title: SpA Including PsA – Diagnosis, Manifestations, & Outcomes Poster I
Session Type: Poster Session A
Session Time: 10:30AM-12:30PM
Background/Purpose: Patients with axial spondyloarthritis (axSpA) have a heightened risk of cardiovascular morbidity and mortality. Nonsteroidal anti-inflammatory drugs (NSAIDs) are first line treatment for axSpA, their potential to elevate blood pressure and exacerbate cardiovascular risk may curtail their sustained usage. We evaluated the relation between NSAID use and incident hypertension in a longitudinal inception cohort of patients with axSpA.
Methods: We studied data from a longitudinal French cohort of early spondyloarthritis (DEvenir des Spondylarthopathies Indifférenciées Récentes [DESIR]) with 72-month follow-up. Participants were followed up every 6 months for the first 2 years, then yearly. We excluded participants with an alternative diagnosis (other than axSpA) on follow-up (n=45) and prevalent cases of hypertension at baseline (n=32). Hypertension was defined with self-reported diagnosis, anti-hypertensive medication use, or systolic blood pressure (BP) ≥ 140 mmHg or diastolic BP ≥ 90 mmHg on ≥2 visits. NSAID usage during the prior 6 months was quantified using the ASAS NSAID index at each visit, and categorized as high (≥50) or low dose . To study the relationship between time varying NSAID use and incident hypertension longitudinally, we used Cox proportional hazards models. We sequentially adjusted for potential confounders in three models: age (Model 1), baseline factors including comorbidities (Model 2), and time-varying covariates including disease activity and medication use (Model 3). We used multiple imputation with chained equations for missing data and compared results to complete case analyses.
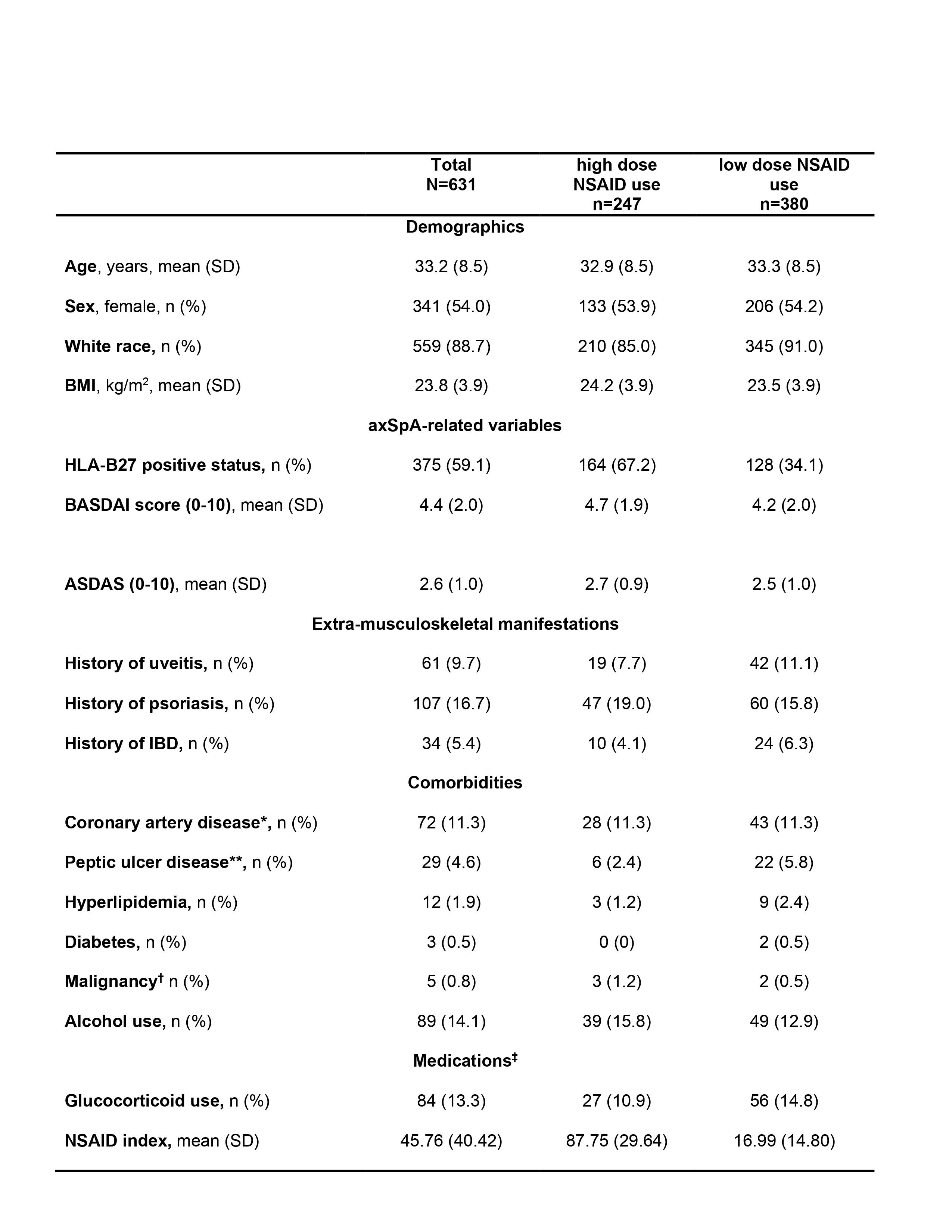
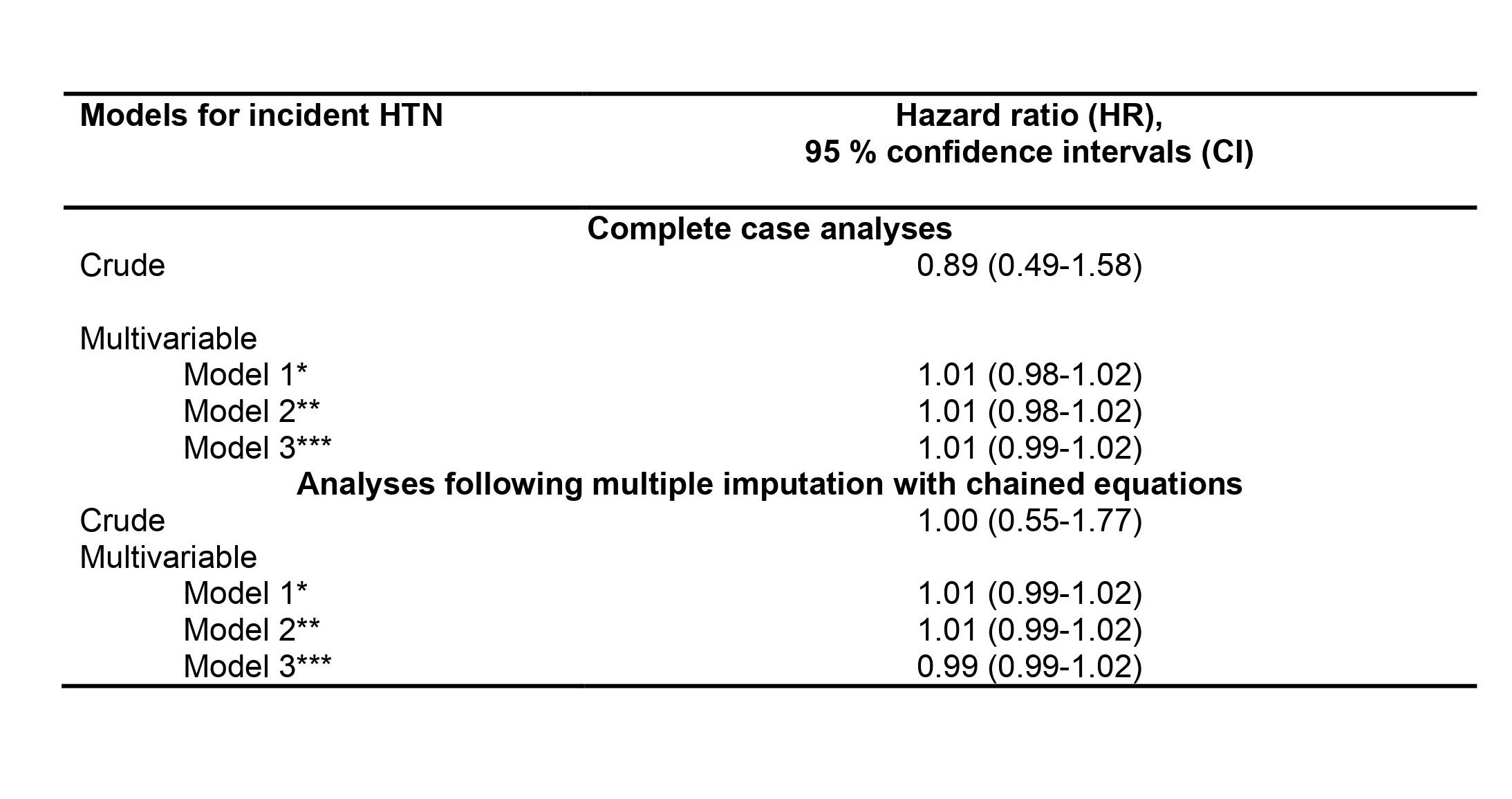
Results: We included 631 participants with axSpA (mean age at baseline 33.2 (8.5) years; 54% female, 89% white (Table 1)). Two thirds were high dose NSAID users at baseline. Incident hypertension occurred in 70 (11%) individuals during follow-up. After adjustment for confounders, high dose NSAID use was not associated with incident hypertension (HR 1.01, 95% CI 0.98-1.02) (Table 2). Results were similar following multiple imputation and for complete case analyses.
Conclusion: In this axSpA inception cohort, we found no significant association between high dose NSAID use and the development of hypertension. The anti-inflammatory effects of NSAIDs on disease activity might counterbalance the risk of incident hypertension that is known to occur in the general population.
Abbreviations: BMI: Body mass index; CRP: C-reactive protein; ASDAS: Axial Spondyloarthritis Disease Activity Score; BASDAI: Bath Ankylosing Spondylitis Disease Activity Index; HLA-B27: Human Leukocyte antigen-B27; IBD: Inflammatory Bowel Disease; TNF: Tumor Necrosis Factor.
Missing data (number of subjects, n): NSAID use: 4; Race-Ethnicity: 1; BASDAI score: 2; ASDAS: 4; Alcohol Use: 1; hyperlipidemia:1.
* Coronary artery disease was patient-reported and included ischemia, coronary artery disease and cerebrovascular disease
** Peptic ulcer disease was patient-reported and included perforation, ulcers, and dyspepsia
† Including lymphoproliferative disorders
‡ Medication use was reported as any use for the 6 months prior to the baseline visit
Caption: The exposure (NSAID use) was time-varying in all Cox models.
*Model 1 adjusted by age
**Model 2 adjusted for baseline covariates of age, sex, race/ethnicity, cardiovascular comorbidities, gastrointestinal comorbidities, diabetes
**Model 3 additionally adjusted for time-varying covariates of body mass index, BASDAI score, TNFi usage, steroid usage
To cite this abstract in AMA style:
Meade Aguilar J, Liew J, Stovall R, Ramiro S, Gensler L. Nonsteroidal Anti-Inflammatory Drug Use and Incident Hypertension Among Patients with Axial Spondyloarthritis [abstract]. Arthritis Rheumatol. 2024; 76 (suppl 9). https://acrabstracts.org/abstract/nonsteroidal-anti-inflammatory-drug-use-and-incident-hypertension-among-patients-with-axial-spondyloarthritis/. Accessed .« Back to ACR Convergence 2024
ACR Meeting Abstracts - https://acrabstracts.org/abstract/nonsteroidal-anti-inflammatory-drug-use-and-incident-hypertension-among-patients-with-axial-spondyloarthritis/