Session Information
Date: Friday, November 6, 2020
Title: RA – Diagnosis, Manifestations, & Outcomes II: The Heart of the Matter (0484–0488)
Session Type: Abstract Session
Session Time: 4:00PM-4:50PM
Background/Purpose: RA patients with low body weight incur higher mortality than obese patients. Paradoxically, RA patients in the lowest low-density lipoprotein group (LDL < 70 mg/dl) also experience unexpectedly high cardiovascular disease (CVD) risk. We here explored whether abdominal obesity (waist-to-height ratio >0.58 in females and >0.63 in males) might moderate the effect of low LDL (< 70mg/dl) on coronary atherosclerosis burden, progression and long-term CVD event risk in RA.
Methods: One hundred fifty patients without symptoms or diagnosis of CVD underwent coronary computed tomography angiography. Plaque progression was evaluated 6.9±0.3 years later in 101 patients. Coronary artery calcium, number of segments with plaque (segment involvement score), and extensive ( >4 segments with plaque) or obstructive disease ( >50% stenosis) were assessed. CVD events were prospectively recorded, including cardiac death, myocardial infarction, unstable angina, revascularization, stroke, claudication, and heart failure hospitalization over 6.0±2.4 years of follow-up. Lipoprotein classes were directly measured. Oxidized LDL (oxLDL) was assessed with monoclonal antibody E06. Adjusted robust linear regression evaluated interactions between abdominal obesity and LDL groups on plaque outcomes. Per segment, adjusted robust logistic regression models explored obesity x LDL group interactions on new plaque formation and stenotic progression of prevalent plaques. Robust Cox regression models stratified by abdominal obesity evaluated the effect of LDL group (< 70 vs. >70mg/dl) on CVD events.
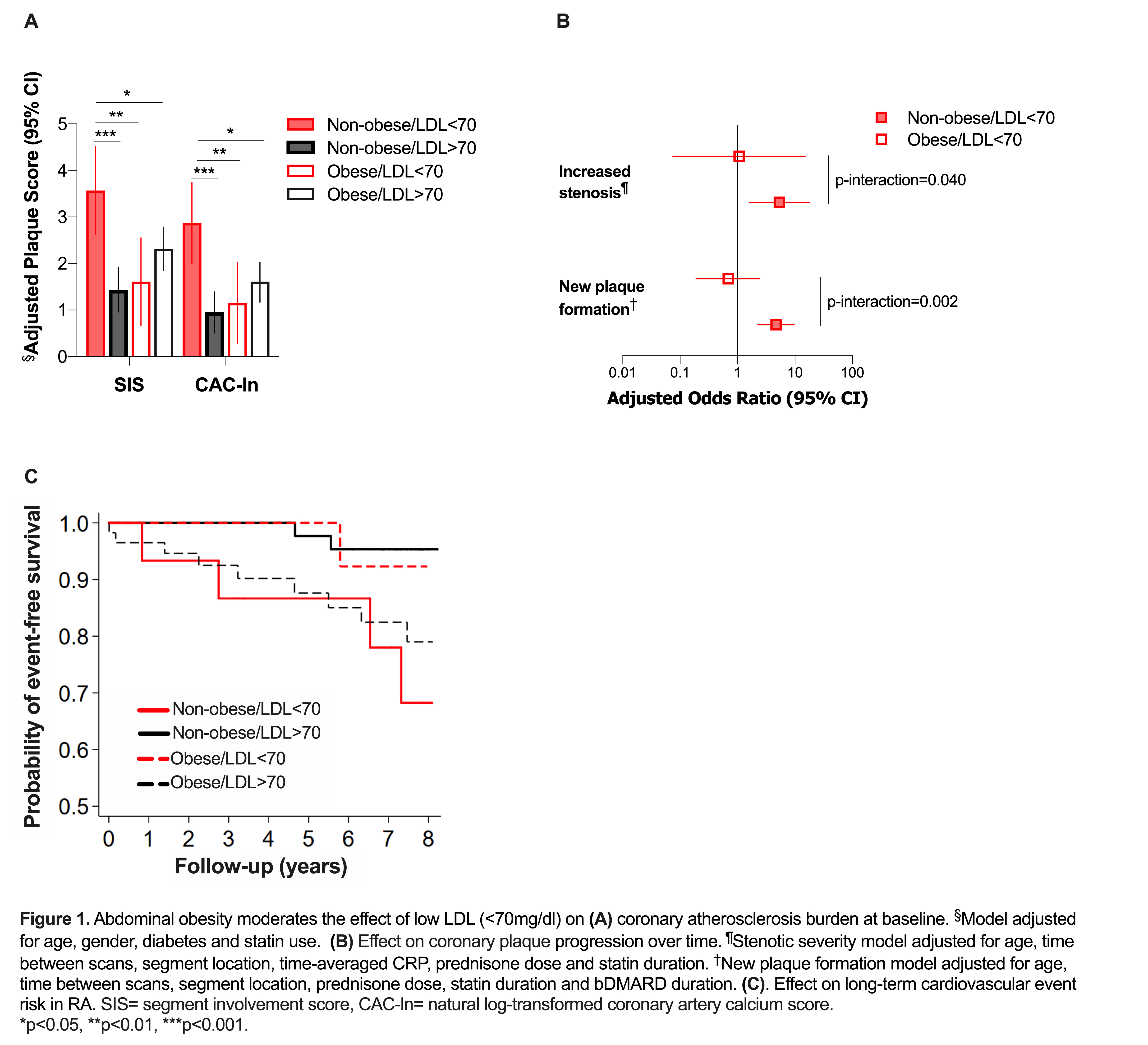
Results: Non-obese patients with low LDL had the highest plaque burden (Figure 1A, all p < 0.02). Obesity further moderated the effect of LDL on likelihood of extensive/obstructive disease (P for interaction = 0.061); specifically, LDL< 70 associated with an increased likelihood of extensive/obstructive plaque in non-obese (adjusted OR 4.75 [95% CI 1.18-19.07], P = 0.028) but not obese patients (adjusted OR 1.55 [95% CI 0.39-6.08], P = 0.532). No differences in disease activity or inflammatory markers were seen across groups. Compared to LDL >70 mg/dl, low LDL predicted an increased likelihood of high oxLDL ( >median) in non-obese patients (adjusted OR 5.10 [95% CI 1.46-17.75], P = 0.011) but not obese patients (adjusted OR 0.50 [95% CI 0.11-2.21], P = 0.36). In non-obese patients, low LDL further associated with a greater likelihood of plaque forming in coronary segments without baseline plaque (adjusted OR 4.68 [95% CI 2.26-9.66], P < 0.001) and worsening stenotic severity in segments with prevalent plaque (OR 5.35 [95% CI 1.62-17.67], P = 0.006). This was not observed in obese patients (Figure 1B). Notably, in non-obese patients, low LDL associated with higher CVD event risk compared to those with LDL >70 mg/dl (HR 7.94 [95% CI 1.52-41.36], P = 0.015). This was not the case in obese patients (HR 0.32 [95% CI 0.04-2.40], P= 0.27, Figure 1C).
Conclusion: In non-obese RA patients, LDL< 70 mg/dl may reflect higher LDL oxidation and was associated with higher baseline coronary atherosclerosis burden, new plaque formation, stenotic plaque progression and greater CVD risk than LDL >70 mg/dl.
To cite this abstract in AMA style:
Karpouzas G, Ormseth S, Hernandez E, Budoff M. Non-obese Rheumatoid Arthritis Patients with Low Low-density Lipoprotein Have Higher Coronary Atherosclerosis Burden, Greater Plaque Progression and Cardiovascular Event Risk [abstract]. Arthritis Rheumatol. 2020; 72 (suppl 10). https://acrabstracts.org/abstract/non-obese-rheumatoid-arthritis-patients-with-low-low-density-lipoprotein-have-higher-coronary-atherosclerosis-burden-greater-plaque-progression-and-cardiovascular-event-risk/. Accessed .« Back to ACR Convergence 2020
ACR Meeting Abstracts - https://acrabstracts.org/abstract/non-obese-rheumatoid-arthritis-patients-with-low-low-density-lipoprotein-have-higher-coronary-atherosclerosis-burden-greater-plaque-progression-and-cardiovascular-event-risk/