Session Information
Session Type: Poster Session A
Session Time: 8:30AM-10:30AM
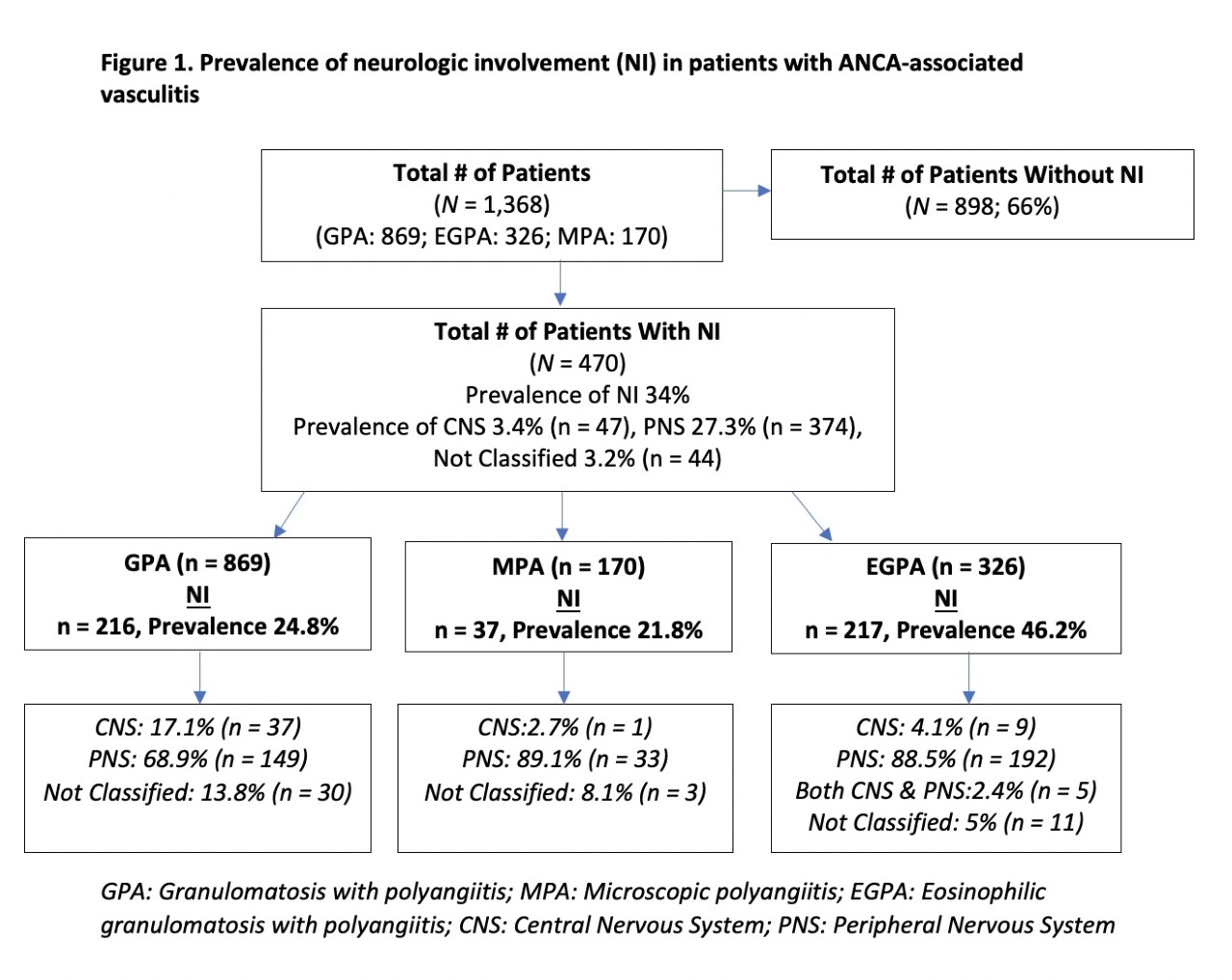
Background/Purpose: The prevalence of neurologic involvement (NI) in ANCA-associated vasculitis (AAV), especially central nervous system (CNS) involvement, is not well characterized. This project aimed to describe the prevalence and types of peripheral nervous system (PNS) NI and CNS NI in AAV, and associations of NI with other manifestation of vasculitis.
Methods: Analysis of patients with AAV [granulomatosis with polyangiitis (GPA), microscopic polyangiitis (MPA), or eosinophilic granulomatosis with polyangiitis (EGPA)] participating in a multicenter longitudinal observational study. Data were from 2006-2021 from patients at least 18 years old at enrollment. Standardized forms were used to document patient demographics, disease type, organ involvement, and ANCA status. Patient subsets were compared according to presence or absence of NI.
Results: Data from 1368 patients were available: 470 (34%) had NI (Figure 1) of whom 216 (46%) had GPA, 37 (7.8%) had MPA, and 217 (46.2%) had EGPA. The prevalence of NI was 24.8% (216/869) in GPA, 22% (37/170) in MPA, and 67% (217/326) in EGPA. The prevalence of CNS NI in the total cohort was 47/1368 (3.4%) and the prevalence of PNS NI was 374/1368 (27.3%), with 44 patients (3.2%) having NI that was not classified. GPA was the most common diagnosis in patients with CNS NI (78% compared to 2% in MPA and 19% in EGPA). For PNS NI, EGPA was the most common diagnosis (51% compared to 40% in GPA and 8.8% in MPA).
Patient sex and race did not differ between patients with or without NI. Patients with NI were 53% female and 47% male, 88.7% were White, 1.5 % Black, 3.2% Hispanic, and 4.8% Asian. Mean age at diagnosis of patients with NI was higher than patients without NI (51.4 vs 47.0 years, p <0.001). NI was associated with skin (49.4% vs. 29.5%, p < 0.001), venous thrombosis (12.8% vs. 8.6%, p= 0.016), and cardiovascular (15.5% vs. 7.2%, p < 0.001) involvement. Patients with NI were less likely to have renal (45.6% vs. 55.9%, p < 0.001), and eye (20 % vs. 28%, p < 0.001) involvement. NI was associated with skin and kidney involvement in EGPA, musculoskeletal, skin, kidney, venous thromboses in GPA and constitutional and musculoskeletal symptoms in MPA (Figure 2).
Patients with NI were more likely to have P-ANCA pattern (43.1 % vs 31.2 % p =0008) and anti-MPO (44.4% vs 30% p < .0001) than patients with no NI.
Conclusion: NI in AAV is common, occurring in approximately one-third of patients, and was most common in EGPA, compared to GPA or MPA. CNS NI occurs more commonly in GPA. NI is associated with various specific organ systems and P-ANCA/anti MPO positivity. These data are informative for clinicians and patients with AAV, and should raise the awareness of this common manifestation of vasculitis. The relationships of NI with other specific manifestations of disease warrants additional study.
To cite this abstract in AMA style:
Hajj-Ali R, Butler R, Langford C, Calabrese L, Cuthbertson D, Khalidi N, KOENING C, McAlear C, Monach P, Moreland L, Pagnoux C, Seo P, Specks U, Sreih A, Warrington K, Merkel P. Neurologic Involvement in ANCA-associated Vasculitis: Data from Multicenter Longitudinal Observational Study [abstract]. Arthritis Rheumatol. 2021; 73 (suppl 9). https://acrabstracts.org/abstract/neurologic-involvement-in-anca-associated-vasculitis-data-from-multicenter-longitudinal-observational-study/. Accessed .« Back to ACR Convergence 2021
ACR Meeting Abstracts - https://acrabstracts.org/abstract/neurologic-involvement-in-anca-associated-vasculitis-data-from-multicenter-longitudinal-observational-study/