Session Information
Session Type: Abstract Session
Session Time: 10:30AM-11:30AM
Background/Purpose: Musculoskeletal Ultrasound (MSUS) has become widely used in rheumatology practice for diagnosis of arthritis and procedural guidance. A 2017 survey of adult rheumatology fellowship programs in the United States (US) reports that 94% provide MSUS training. In contrast, a 2014 survey of US pediatric rheumatology fellows shows that only 20% receive formal MSUS training. MSUS is advantageous in pediatrics as it does not require radiation or sedation. This study aims to assess interest in, access to, and barriers to MSUS training in pediatric rheumatology fellowship programs in North America.
Methods: A survey was developed by pediatric rheumatology providers with experience in medical and/or MSUS education and refined through 7 cognitive interviews. The questions focused on fellows’ interest in, access/barriers to MSUS training, and program support. Eligible participants included current and recently graduated (< 1 year) pediatric rheumatology fellows at a North American program. REDCap was used to distribute the anonymous survey electronically in March 2022. Descriptive statistics and bivariate analyses using Design-Based Pearson Chi-Squared tests to account for clustering of fellows by institution were performed. Nonresponse bias analyses indicated a low likelihood for bias.
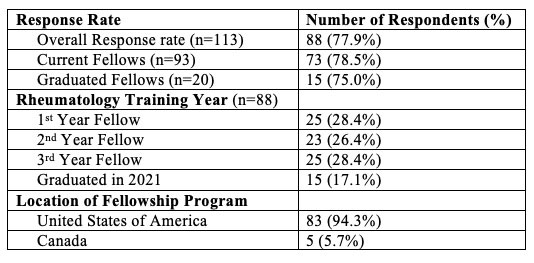
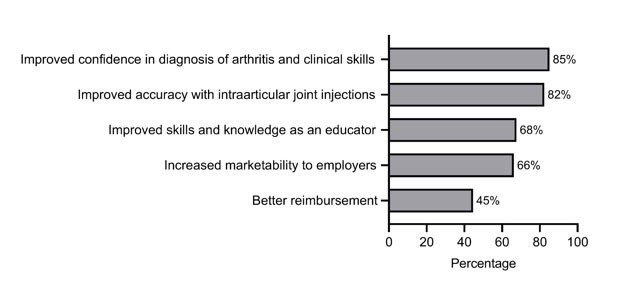
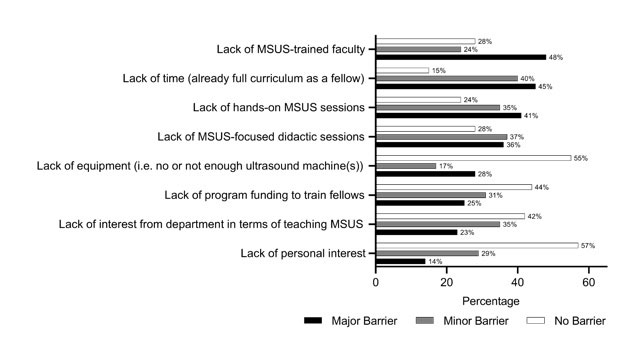
Results: Overall response rate was 78% (88/113) (Table 1). Sixty-eight percent of respondents reported some form of MSUS training, and 86% reported interest in learning MSUS during fellowship. Similarly, 84% of respondents felt MSUS would be beneficial to their career, citing improved confidence in diagnosis of arthritis and clinical skills (85%) as well as improved accuracy with joint injections (82%) as potential benefits (Figure 1). Fourteen percent did not see benefit in MSUS for their career, with the greatest perceived barrier being lack of time (50%). Of those with MSUS training, 23% reported adult-only MSUS education. Only 36% of respondents indicated their program had a formal MSUS curriculum. Two-thirds (63%) of respondents felt that MSUS training should be formally included as part of the pediatric rheumatology fellowship curriculum. Major barriers to MSUS training during fellowship included lack of MSUS-trained faculty (48%), lack of time (45%), and lack of hands-on MSUS sessions (41%) (Figure 2). Those who had access to MSUS training were significantly more interested in MSUS than those without (p=0.004).
Conclusion: This study demonstrates that North American pediatric rheumatology fellows have a strong interest in learning MSUS, but they face significant limitations in accessing MSUS training. Perceived barriers include lack of MSUS-trained faculty, time and access to hands-on training. Fellows and recent graduates with MSUS training during fellowship had greater interest in MSUS compared to those without. This suggests MSUS exposure during fellowship plays a key role in garnering interest and filling the need for more MSUS-trained faculty. MSUS training is of value to pediatric rheumatology fellows and should be incorporated into fellowship curriculum, however, implementation remains a challenge.
To cite this abstract in AMA style:
Perron M, Ziniel S, Curran M, Bloom J, Vega-Fernandez P, Benham H, Torralba K, De Ranieri D, Lin C. Needs Assessment of Musculoskeletal Ultrasound Training in North American Pediatric Rheumatology Fellowship Programs [abstract]. Arthritis Rheumatol. 2022; 74 (suppl 9). https://acrabstracts.org/abstract/needs-assessment-of-musculoskeletal-ultrasound-training-in-north-american-pediatric-rheumatology-fellowship-programs/. Accessed .« Back to ACR Convergence 2022
ACR Meeting Abstracts - https://acrabstracts.org/abstract/needs-assessment-of-musculoskeletal-ultrasound-training-in-north-american-pediatric-rheumatology-fellowship-programs/