Session Information
Date: Tuesday, October 28, 2025
Title: (1972–1989) Measures & Measurement of Healthcare Quality Poster II
Session Type: Poster Session C
Session Time: 10:30AM-12:30PM
Background/Purpose: Young adults with childhood-onset rheumatic conditions encounter challenges and barriers to care when transitioning to an adult rheumatologist. At this Pediatric Rheumatology Clinic, patients aged 18 and older were provided with a list of adult providers to call and set up follow-up, however no formal transition process existed. This study aimed to pilot the practice’s first program to systematically transition pediatric patients using aspects of the Six Core Elements of Health Care Transition (HCT) from Got Transition.
Methods: One research assistant, two primary care physicians, one pediatric and ten adult rheumatology providers facilitated the program. Patients were eligible if they were 18 years of age or older with confirmed rheumatic disease, and deemed stable to transition by the pediatric rheumatologist. The program structure consisted of four visits, ~three months apart: two appointments with pediatric rheumatology, with ~50% of the time devoted to transition readiness education; a final in-person appointment with pediatric rheumatology, with their chosen adult rheumatologist on video for a warm handoff; and a first appointment with adult rheumatology. Patient-reported transition readiness was assessed at each visit using the Transition Readiness Assessment (TRA) from Got Transition. Patient demographics were assessed via chart review.
Results: 64 patients aged 18 and older had scheduled appointments with the Pediatric Rheumatology Clinic from 5/1/24 to 1/31/25. Of these patients, 13 were eligible, determined by diagnosis and disease stability, of which eight (62.5%) chose to enter the pilot (Figure 1). Patient demographics are shown in Table 1.All participants (100%) completed a baseline TRA. The mean age at enrollment was 19.5 years (range: 18-23). Mean TRA scores for patients’ initial self-perceived importance of transition to an adult doctor and confidence in transitioning were 8.13 and 7.13, respectively (out of 0 [not] to 10 [very]). The majority of participants reported knowing their health needs and being able to explain them to others. Knowledge regarding navigating health care, such as getting referrals to other providers, was more mixed (Figure 2). Seven participants (87.5%) have completed at least two transition appointments, and two (25%) have successfully transitioned to adult rheumatology.
Conclusion: Appropriate HCT is crucial to support the health of young adults with childhood-onset chronic illnesses. Initial stages of this transition process have proven acceptable with the majority of patients approached agreeing to participate. It appears that self-perceived importance of transitioning to an adult rheumatologist was greater than confidence in doing so at the initial appointment. It has also proven feasible to complete successful warm video handoff visits with the adult rheumatologists at their final pediatric appointment. Challenges to implementation include time and clinical infrastructure. Next steps involve finalizing remaining adult appointments and assessing the impact of this program on patients with multi-modal data – qualitative and quantitative surveys.
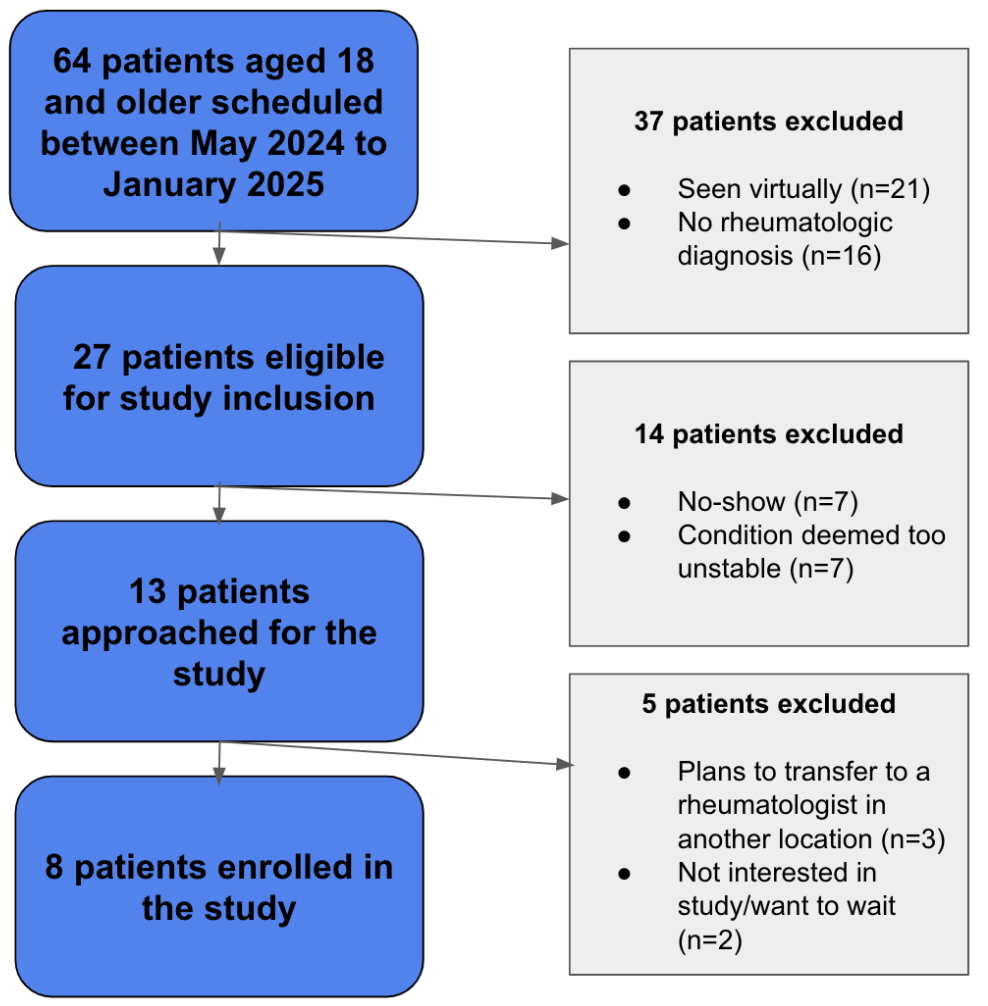 Table 1: Participant Demographics
Table 1: Participant Demographics
.jpg) Figure 1: Participant Enrollment
Figure 1: Participant Enrollment
.jpg) Figure 2: Baseline Transition Readiness (TRA) Responses
Figure 2: Baseline Transition Readiness (TRA) Responses
To cite this abstract in AMA style:
Koenigsberger V, Ward M, Geary M, Yalcindag A. Moving Out of the Kid’s Rheum: Transitioning Young Adult Patients from Pediatric to Adult Rheumatology Practices [abstract]. Arthritis Rheumatol. 2025; 77 (suppl 9). https://acrabstracts.org/abstract/moving-out-of-the-kids-rheum-transitioning-young-adult-patients-from-pediatric-to-adult-rheumatology-practices/. Accessed .« Back to ACR Convergence 2025
ACR Meeting Abstracts - https://acrabstracts.org/abstract/moving-out-of-the-kids-rheum-transitioning-young-adult-patients-from-pediatric-to-adult-rheumatology-practices/
