Session Information
Session Type: Poster Session A
Session Time: 9:00AM-11:00AM
Background/Purpose: Systemic autoimmune diseases (sAIDs) have become leading contributors to premature death. Meanwhile, regional disparities exist in capacity of rheumatology healthcare services delivery. However, no rigorous epidemiological studies have provided an integrated overview of mortality burden of various sAIDs, especially in low-to-middle income countries (LMICs). In this study, we comprehensively analyzed mortality rates, survival probabilities, causes of death, and standardized mortality ratios (SMRs) of eight sAIDs in China and examined the associations between disease burden of sAIDs and development indicators.
Methods: In this nationwide, register-based cohort study, we used data from Chinese Rheumatism Data Center, Nation Mortality Surveillance System, and public databases with a universal coverage of 31 provinces in mainland China between Jan 1, 2011, and Dec 31, 2021. We collected data on patient demographics, clinical status, and vital outcomes of individuals with RA, SLE, SS, IIM, SSc, Behçet’s disease (BD), Takayasu’s arteritis (TAK), and AAV. Mortality rates, survival probabilities, causes of death, and SMRs were estimated in patients classified by gender, age at disease onset, and area-level socioeconomic status (including a composite indicator, human development index [HDI], and indicators in economy, healthcare, and education).
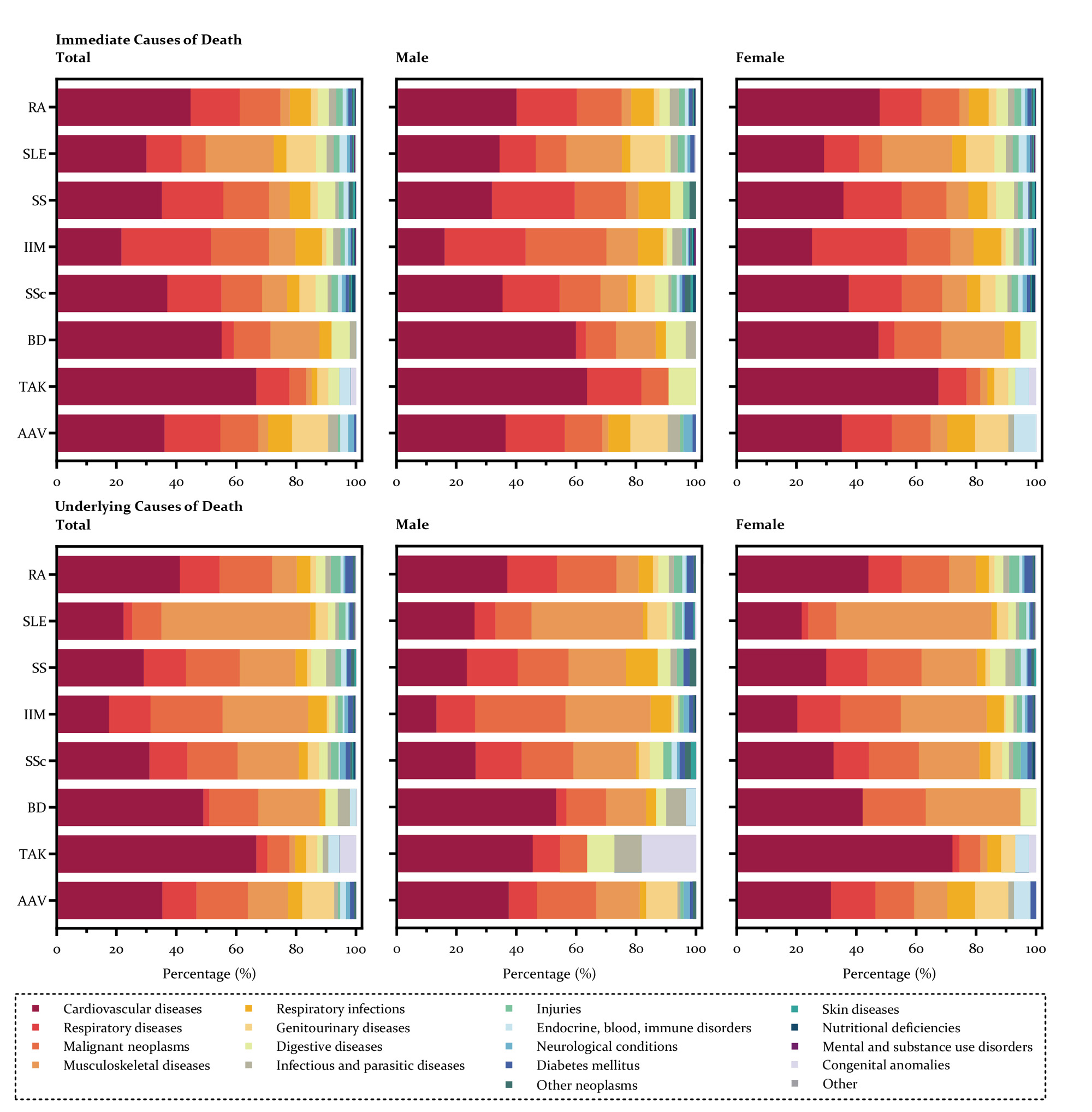
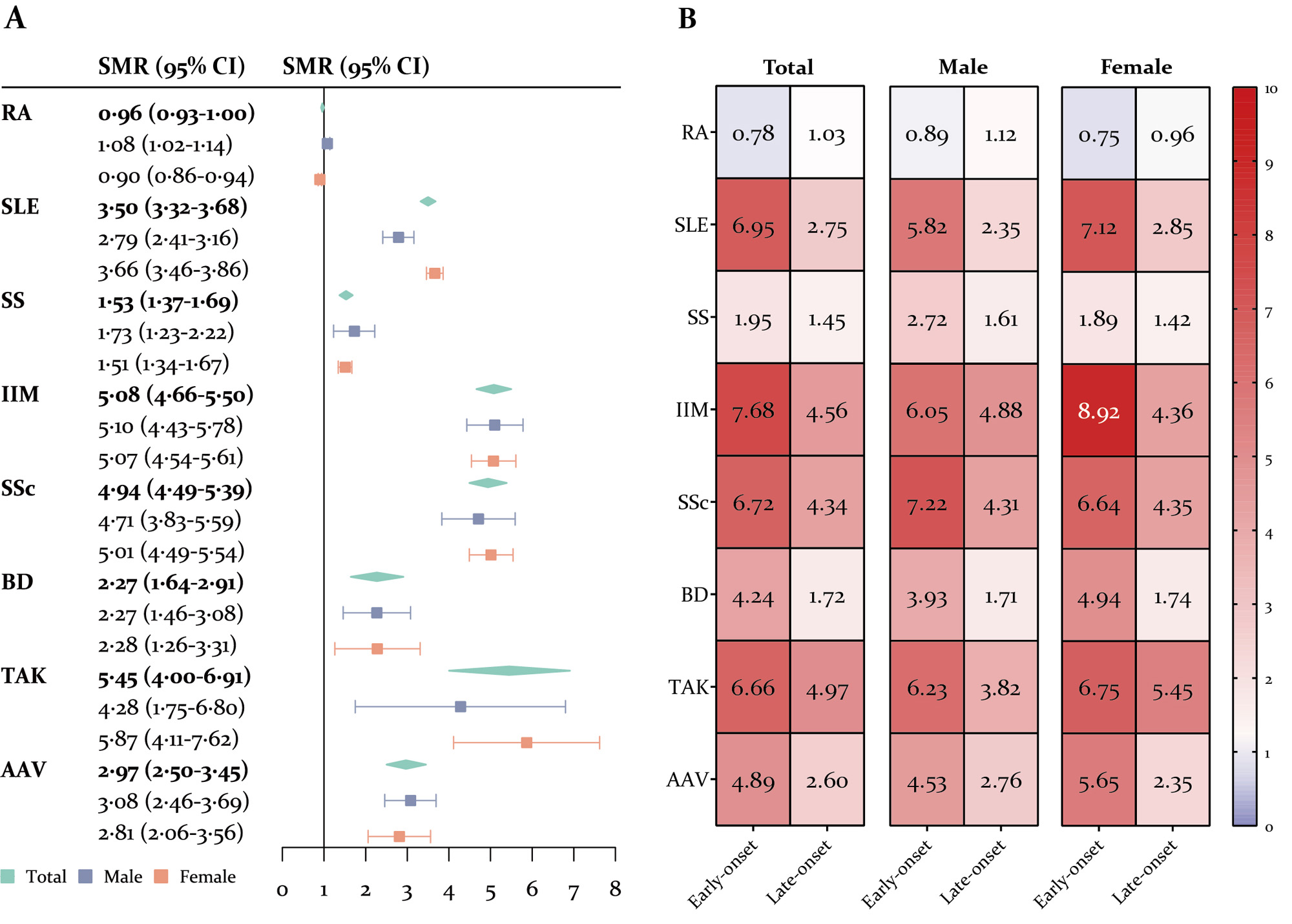
Results: Between 2011 and 2021, 156 862 individuals (87132 with RA, 44658 with SLE, 11668 with SS, 4864 with IIM, 4065 with SSc, 1762 with BD, 1558 with TAK, and 1155 with AAV) were included, with a median duration of follow-up 5.12 (IQR 3.08-8.67) years. AAV, IIM, and SSc were top three diseases with the highest fatality rates and lowest survival rates. Cardiovascular, respiratory (non-infection), musculoskeletal, malignancy, and genitourinary diseases were the leading causes of death (Figure 1). The age-, gender-, and calendar year-adjusted SMR was highest for TAK (5.45, 95%CI 4.00-6.91), followed by IIM (5.08, 4.66-5.50), SSc (4.94, 4.49-5.39), SLE (3.50, 3.32-3.68), AAV (2.97, 2.50-3.45), BD (2.27, 1.64-2.91), SS (1.53, 1.37-1.69), and RA (0.96, 0.93-1.00). Early disease-onset is a risk factor of excess death in patients with sAIDs (Figure 2). Additionally, higher HDI was associated with significant increases in mortality risks in both RA and SLE (SMR ratio 12.24 and 5.15 for 1-unit increase in HDI, p< 0.001 and p=0.080) patients compared with region-specific general population. More medical institutions (SMR ratio 0.95 for one more medical institution per 10 000 resident population, p=0.005) and hospital beds (SMR ratio 0.35 for one more hospital bed per 100 resident population, p=0.131) were protect factors of excess mortality in SLE.
Conclusion: The mortality risk in patients with sAIDs can be in substantial excess versus general population, and sAIDs are becoming important contributors to premature mortality in China. Increasing mortality burden associated with sAIDs implied the relative insufficiency of capacity building of diagnosis and treatment in sAIDs in LMICs, raising important need for establishing universal health coverage systems for the affected patients.
To cite this abstract in AMA style:
Li M, Wu C, Yin P, Wang Q, Xu D, Leng X, Tian X, Duarte-Garcia A, Li M, Zeng x, Zhou M. Mortality-related Health Metrics in Systemic Autoimmune Diseases: An Epidemiological Analysis of a Nationwide Register-based Cohort [abstract]. Arthritis Rheumatol. 2023; 75 (suppl 9). https://acrabstracts.org/abstract/mortality-related-health-metrics-in-systemic-autoimmune-diseases-an-epidemiological-analysis-of-a-nationwide-register-based-cohort/. Accessed .« Back to ACR Convergence 2023
ACR Meeting Abstracts - https://acrabstracts.org/abstract/mortality-related-health-metrics-in-systemic-autoimmune-diseases-an-epidemiological-analysis-of-a-nationwide-register-based-cohort/