Session Information
Date: Sunday, October 26, 2025
Title: Abstracts: Pain in Rheumatic Disease Including Fibromyalgia (0813–0818)
Session Type: Abstract Session
Session Time: 4:00PM-4:15PM
Background/Purpose: Patients with rheumatic diseases commonly experience acute or chronic pain that may lead to both short- and long-term opioid use. Many patients do not experience benefit in function or pain from increasing opioid dosages to ≥50 morphine milligram equivalents (MME)/day but do have increased risks, including dependence or overdose as the dose is increased. We used national data from the Rheumatology Informatics System for Effectiveness (RISE) registry linked to Medicare claims to quantify the prevalence and risk factors of receiving opioids including high dose prescriptions (Rx’s) among older adults with rheumatic conditions associated with pain.
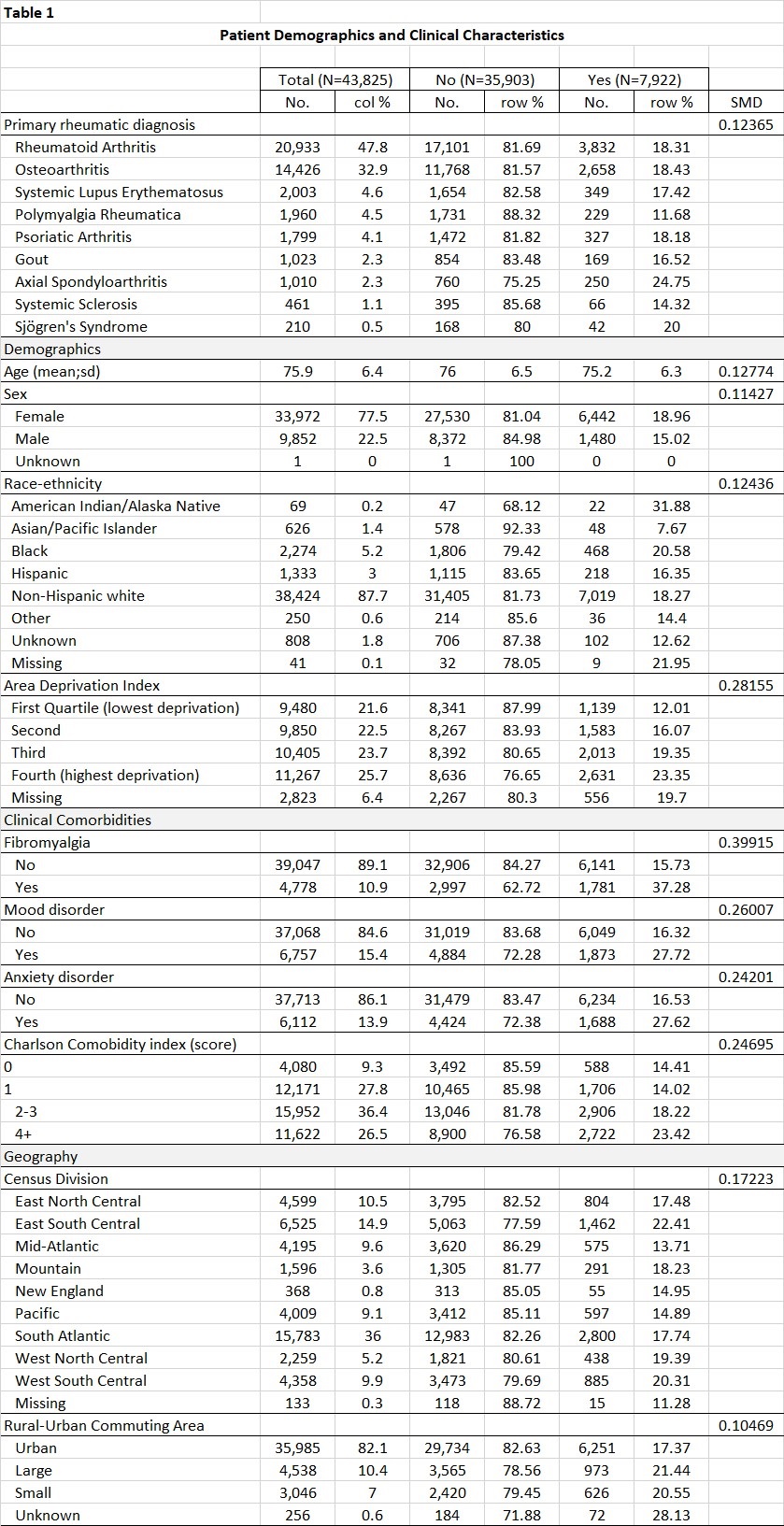
Methods: Adults ≥65 years old with ≥2 visits to a RISE practice in 2021, continuous Medicare enrollment (Parts A, B, & D) in 2021, and at least one rheumatic diagnosis of RA, OA, axSpA, SLE, PsA, PMR, SS, SSc, or gout were included. Patients with ≥2 ICD-10 codes for cancer were excluded. Outcomes were evaluated in Medicare claims and included: (1) any opioid dispensation, (2) chronic Rx (≥90 days), (3) max 90-day average morphine equivalent dose (MED), (4) and the MED for each claim was calculated and dichotomized into Rx’s for ≥50 MME per day or less. Prescriber specialty (rheumatologist (rheum), non-rheum physician, rheum affiliated physician assistant (PA)/nurse practitioner (NP) and non-rheum affiliated PA/NP) was determined by linking to National Provider Identifiers (NPIs). We modeled chronic opioid use as a dichotomous outcome using logit linear models using generalized estimating equations to adjust for patients nested within practices.
Results: Among 43,825 patients (mean age 75.9±6.4, 77.5% female, 87.7% non-Hispanic white), 18,991 (43.3%) filled ≥1 opioid Rx (112,791 total claims). Hydrocodone (19.6%), tramadol (19.1%), and oxycodone (12.1%) were the most common opioid Rx’s. Chronic opioid Rx’s were written in 7,922 patients (18.1%) and the mean maximum 90-day dose was 17.1 mg MED. A quarter of patients receiving opioids (23.8%) had Rx’s written only by rheum providers, 13.4% received Rx’s from a mix of rheum and non-rheum providers, and 5.4% were missing the specialty of the provider. Most Rx’s for ≥50 MME per day were prescribed by non-rheum affiliated NPs/PAs and non-Rheum physicians (Table 2). In the adjusted model, patients with axSpA had more than 50% higher odds of chronic opioid Rx’s compared to those with RA (OR 1.51; 95% CI 1.25-1.82) (Table 3). The odds of chronic opioid Rx increased incrementally with worsening patient socioeconomic deprivation; and fibromyalgia, mood disorders, anxiety disorders and higher comorbidity index were all significantly associated with chronic opioid Rx (Table 3).
Conclusion: In this national sample of older adults with rheumatic diseases, 43% received at least one opioid Rx; patients with axSpA were the most likely to receive an opioid Rx. Among patients receiving opioids, high dose Rx ≥50 MME/day were commonly written by both rheum and non-rheum providers. Further research is needed to identify safer pain therapies for these older adults and to develop targeted interventions that reduce potentially inappropriate opioid prescribing.
To cite this abstract in AMA style:
Anastasiou C, Roberts E, Schmajuk g, Yazdany J. More than 40% of Older Adults with Rheumatic Diseases Are Prescribed Opioid Medications [abstract]. Arthritis Rheumatol. 2025; 77 (suppl 9). https://acrabstracts.org/abstract/more-than-40-of-older-adults-with-rheumatic-diseases-are-prescribed-opioid-medications/. Accessed .« Back to ACR Convergence 2025
ACR Meeting Abstracts - https://acrabstracts.org/abstract/more-than-40-of-older-adults-with-rheumatic-diseases-are-prescribed-opioid-medications/

.jpg)
.jpg)