Session Information
Date: Monday, November 14, 2022
Title: Plenary III
Session Type: Plenary Session
Session Time: 11:30AM-1:00PM
Background/Purpose: Despite extensive studies, the relationship between circulating and local immune cells and clinico-pathological features of Immune-Mediated Inflammatory Diseases remains unclear. Recently, synovium-specific cell states have been described by single cell analyses, however their association with clinical outcomes remains unknown.
Methods: RNA-sequencing was performed on RNA extracted from ultrasound-guided synovial biopsies (n=49) and matched peripheral blood samples (n=36) from patients with early (< 12months) untreated RA (EULAR/ACR 2010 criteria). To assess the presence of 18 recently described synovium-specific immune cell states, we calculated module scores using their most expressed genes, and assessed their association with disease outcomes.
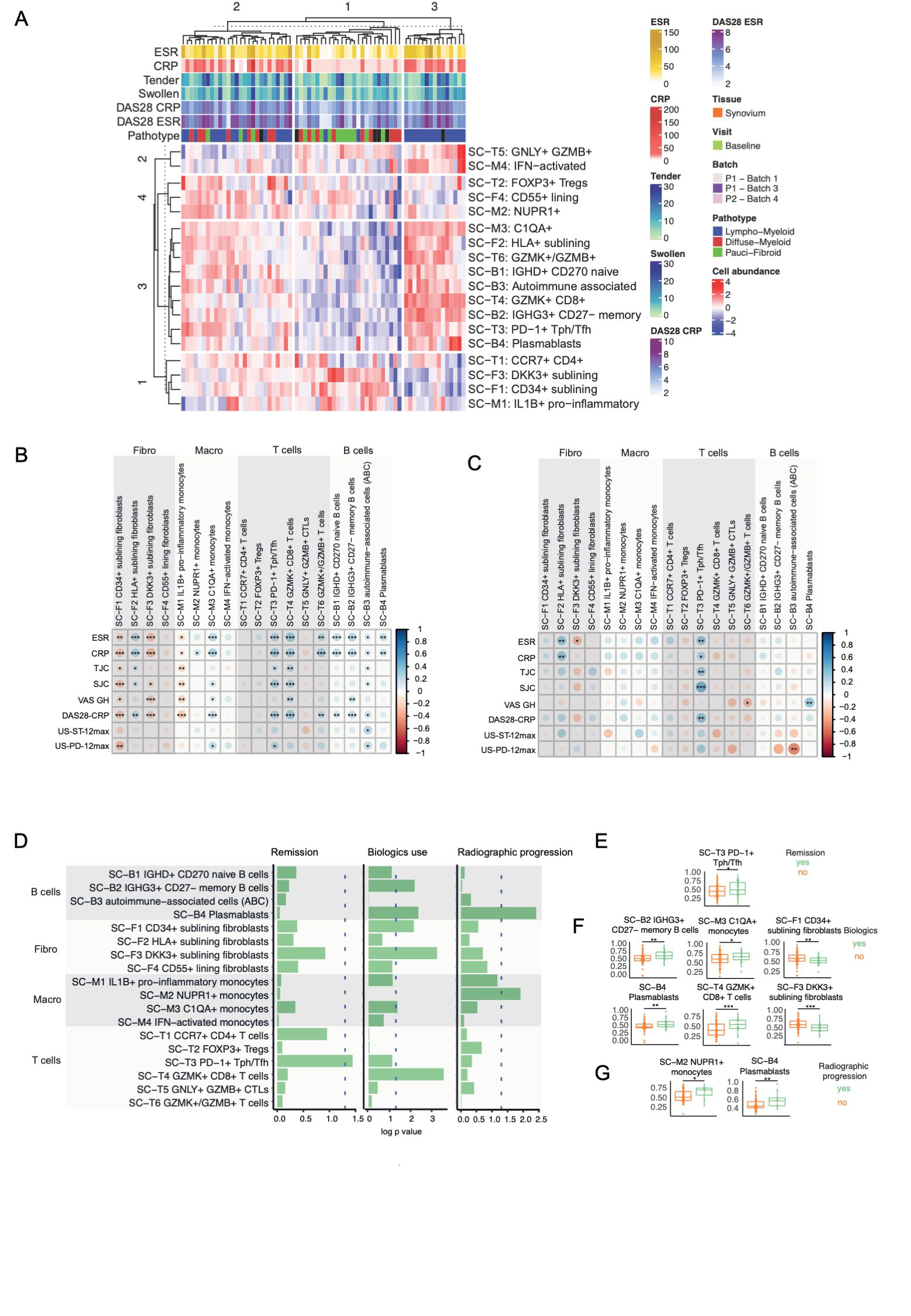
Results: Unsupervised clustering of single-cell module scores identified 3 clusters associated with synovial pathotypes (Figure 1A): cluster 3 corresponding almost exclusively to the lympho-myeloid pathotype, with enrichment of B, T cell and macrophage subsets; cluster 2, with prevalence of the fibroid/pauci-immune pathotype and enrichment of CD34+ sublining fibroblasts, DKK3+ sublining fibroblasts, and IL-1B+ pro-inflammatory macrophages; cluster 1, a mixed group, with a balanced representation of lympho-myeloid and diffuse-myeloid pathotypes/cellular subsets. Further analyses of single-cell signatures revealed a negative correlation of CD34+ sublining fibroblasts, DKK3+ sublining fibroblasts and IL-1B+ pro-inflammatory macrophages with inflammatory markers, tender and swollen joints, and disease activity scores (Figure 1B), while C1QA+ macrophages, PD1+ Tph cells, GZMK+CD8+ T cells and all B cell subsets showed strong positive correlations with inflammatory markers, disease activity and their components (Figure 1B). In the peripheral blood, significant correlations were only maintained for PD1+ Tph cells (Figure 1C). The Tph signature was also associated with clinical outcomes (Figure 1D), as patients reaching remission at 6 months in response to csDMARDs had significantly higher pre-treatment TpH levels (figure 1E). Patients who progressed to biologic DMARDs within 1 year had significantly higher baseline memory B cells (SC-B2 IGHG3+CD27-), plasmablasts, C1QA+ monocytes and GZMK+ CD8 T cells, but significantly lower CD34+ fibroblasts and DKK3+ fibroblasts (Figure 1F). Finally, radiographic progression at 1 year was associated with baseline plasmablast and NUPR1+ monocytes (Figure 1G). These findings were maintained after correcting by logistic regression for baseline demographic and clinical factors.
Conclusion: These results indicate the pre-treatment synovial single-cell modular signatures are associated with disease outcomes, including treatment response, use of biologic DMARDs and structural damage progression.
To cite this abstract in AMA style:
Rivellese F, Pontarini E, Cubuk C, Nerviani A, Fossati-Jimack L, Surace A, Sciacca E, Goldmann K, Bombardieri M, Lewis M, Pitzalis C. Module Signatures of Synovial Single-cell States Identify Disease Phenotypes in Early Treatment-naive Rheumatoid Arthritis [abstract]. Arthritis Rheumatol. 2022; 74 (suppl 9). https://acrabstracts.org/abstract/module-signatures-of-synovial-single-cell-states-identify-disease-phenotypes-in-early-treatment-naive-rheumatoid-arthritis/. Accessed .« Back to ACR Convergence 2022
ACR Meeting Abstracts - https://acrabstracts.org/abstract/module-signatures-of-synovial-single-cell-states-identify-disease-phenotypes-in-early-treatment-naive-rheumatoid-arthritis/