Session Information
Session Type: Poster Session B
Session Time: 10:30AM-12:30PM
Background/Purpose: Interstitial lung disease (ILD) is the main cause of death in systemic sclerosis (SSc). While impaired lung function with forced vital capacity (FVC) < 70% and extensive lung fibrosis by predict excess mortality in SSc, the risk conferred by less advanced ILD is not fully clear. This question has major clinical implications. If even mild SSc-ILD is associated with overall mortality and, more specifically, respiratory causes of death, there is a potential need for aggressive and better-defined management approaches early in the disease. Here, we assessed respiratory causes of deaths in SSc-ILD patients and evaluate the impact of general, SSc-, and lung characteristics on respiratory-caused mortality in patients with preserved lung function.
Methods: The study cohort included SSc-ILD patients (N=323) from the Norwegian SSc cohort who had ILD diagnosed by HRCT, and had prospective clinical data available. The Norwegian national population registry provided vital status for all patients. We obtained causes of death from death certificates and by chart review and segregated them into respiratory and non-respiratory causes. General, SSc-specific, and lung characteristics were determined for associations with respiratory causes of death.The severity of ILD was defined as mild or severe ILD based on lung function (FVC% predicted ≥/< 70%), the extent of ILD on HRCT < /≥10%, and the absence or presence of respiratory symptoms (WHO functional class ≤/ >2). We used logistic regression to assess the impact of characteristics on respiratory-caused mortality in mild ILD based on preserved lung function.
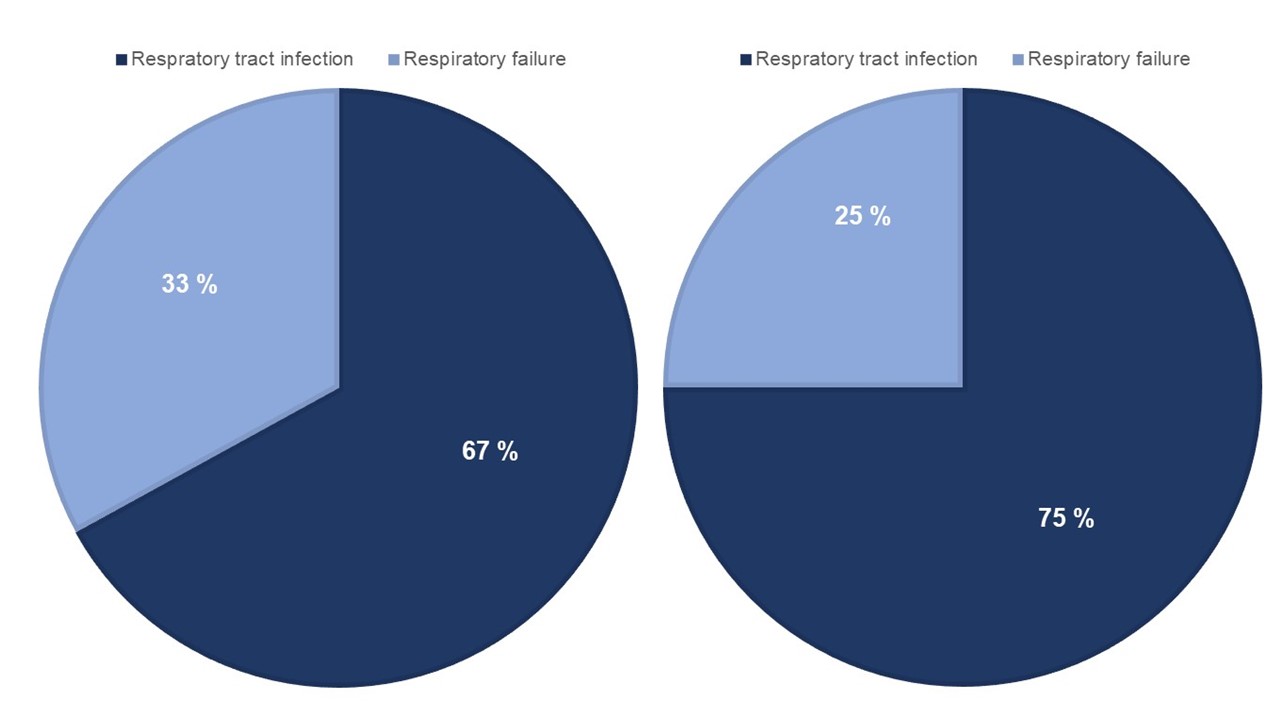
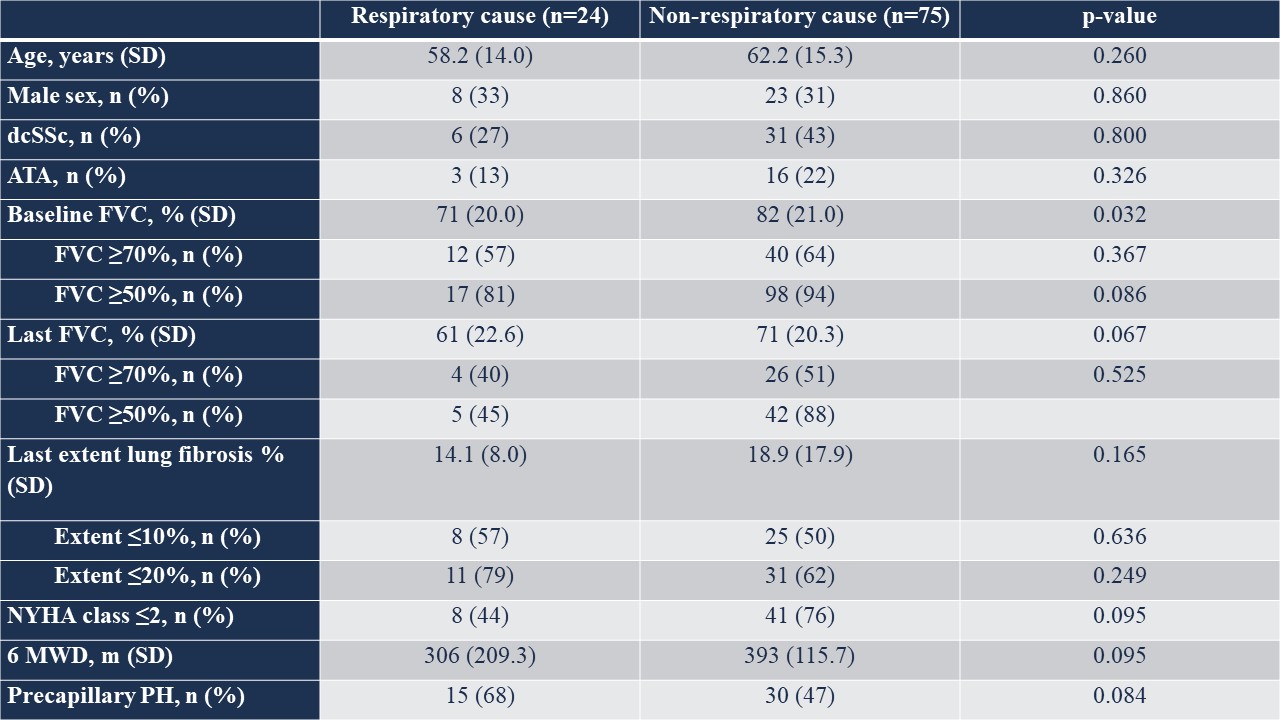
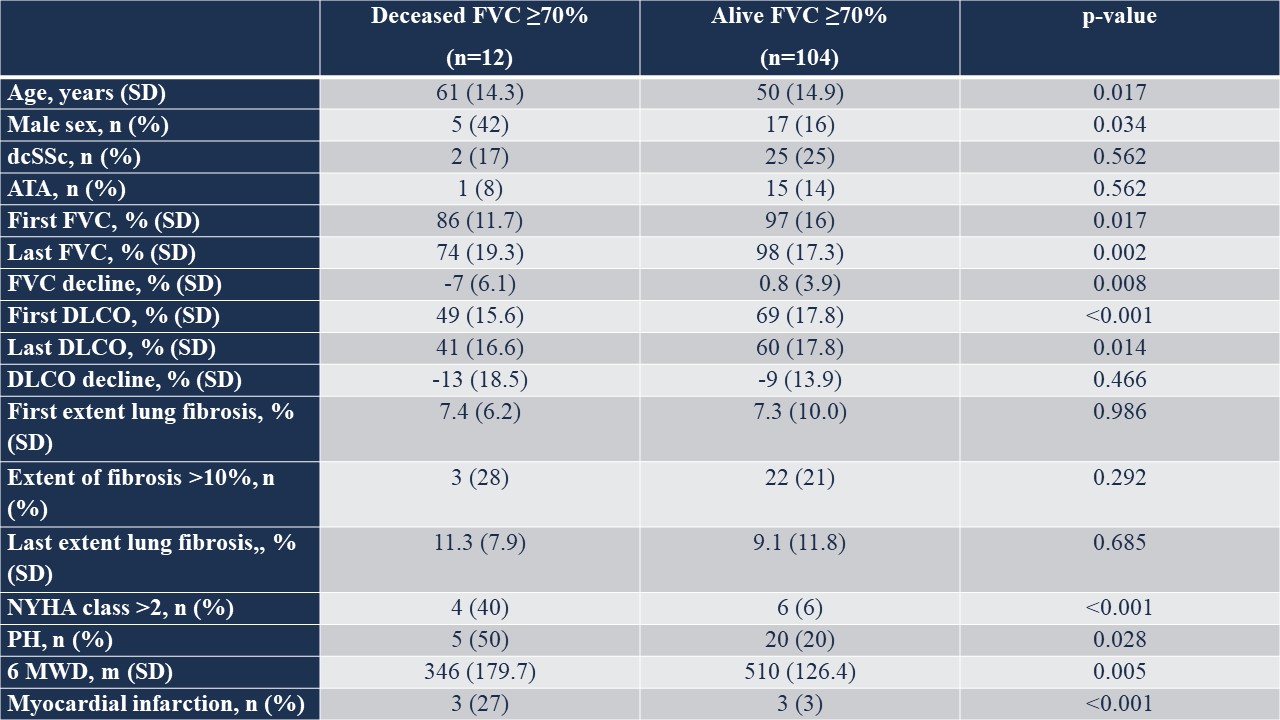
Results: Out of 323 SSc-ILD patients, 132 (41%) were deceased. Causes of death were available for 99 (76%) patients (Table 1A). Of these, 24 (24%) died of respiratory causes, with 67% dying of respiratory tract infections and 33% of respiratory failure (Figure 1A). Among the 24 patients who died of respiratory causes, 50% had FVC ≥70%, 57% had ≤10% extent of ILD on HRCT, and 44% had reported absence of respiratory symptoms mean 1.1 year prior to death (Table 1A). Next, we aimed to identify clinical characteristics of patients dying of respiratory caused mortality with preserved lung function. We compared the characteristics of the 12 SSc-ILD patients with preserved lung function (defined as FVC ≥70%) who died of respiratory causes to 104 surviving peers (Table 1B). We found that older age, male sex, progressive ILD defined as FVC decline, the presence of respiratory symptoms, reduced six-minute walking distance (6MWD), and the development of pulmonary hypertension (PH) were associated with mortality despite preserved lung function (Table 1B). The main cause of respiratory deaths in these patients was respiratory tract infections (75%) (Figure 1B). No specific SSc manifestations were identified to be associated with respiratory-caused mortality (Figure 2).
Conclusion: A significant proportion of SSc-ILD patients who died of respiratory causes had preserved lung function and did not progress to more severe, end-stage lung disease. Our results highlight the importance of preventing the onset of ILD, as well as halting its progression, even in cases of mild ILD, to improve ILD-associated survival in SSc patients.
To cite this abstract in AMA style:
Hoffmann-Vold A, Fretheim H, Langballe E, Jenssen Bjørkekjær H, Didriksen H, Diep P, Andersson A, Gunnarsson R, Durheim M, Garen T, Midtvedt Ø, Aaløkken T, Molberg Ø, Distler O. Milder ILD with Preserved Lung Function Significantly Contributes to Respiratory Caused Mortality in SSc [abstract]. Arthritis Rheumatol. 2024; 76 (suppl 9). https://acrabstracts.org/abstract/milder-ild-with-preserved-lung-function-significantly-contributes-to-respiratory-caused-mortality-in-ssc/. Accessed .« Back to ACR Convergence 2024
ACR Meeting Abstracts - https://acrabstracts.org/abstract/milder-ild-with-preserved-lung-function-significantly-contributes-to-respiratory-caused-mortality-in-ssc/