Session Information
Session Type: Poster Session D
Session Time: 9:00AM-11:00AM
Background/Purpose: Obesity-related metabolic dysregulation may lead to atherosclerotic vascular changes. It has been hypothesized that a compromised blood flow may cause detrimental changes to the subchondral bone and decrease nutrient supply to the cartilage. To which extent atherosclerosis may explain the association between obesity and osteoarthritis has not been investigated. Therefore, we aimed to investigate the role of blood pressure, arterial stiffness (pulse wave velocity (PWV)) and subclinical atherosclerosis (carotid intima-media thickness (IMT), popliteal vessel wall thickness (VWT)) as mediators of the association of obesity with hand and knee osteoarthritis.
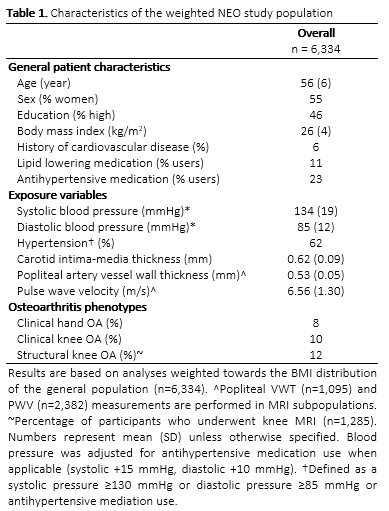
Methods: We used cross-sectional data from the population-based NEO study, excluding participants with concomitant rheumatic diseases (n = 323) and missing physical examination (n = 14), resulting in 6,334 participants. Clinical hand and knee osteoarthritis were defined by the ACR classification criteria. Eight percent of the participants satisfied the ACR classification criteria for hand osteoarthritis, and 10% of participants was classified with clinical knee osteoarthritis. Structural knee osteoarthritis was assessed on MRI in a subpopulation (n = 1,285). Popliteal VWT was assessed on MRI (n = 1,095), using VesselMASS for semi-automated detection of the vessel wall boundaries. Aortic PWV was estimated on abdominal velocity-encoded MRI (n = 2,580). Carotid IMT was assessed by ultrasonography in all participants. Blood pressure was corrected for the use of antihypertensive medication (systolic +15 mmHg, diastolic +10 mmHg). Continuous variables were standardized (mean 0, standard deviation 1). Associations between BMI and osteoarthritis were assessed with logistic regression analyses, adjusted for age, sex and education. Subsequently, possible mediators were added to the model. The assumptions for mediation according to the Baron and Kenny framework were assessed, and if fulfilled the percentage mediation was calculated.
Results: The population consisted of 55% women, with a mean age of 56 years and BMI of 26 kg/m2. Clinical hand osteoarthritis was present in 8%, clinical knee osteoarthritis in 10% and structural knee osteoarthritis in 12% of participants. Mean blood pressure was 134/85 mmHg. Mean carotid IMT was 0.62 mm, popliteal VWT was 0.53 mm, and PWV was 6.56 m/s (table 1). BMI was positively associated with all osteoarthritis outcomes. Carotid IMT partially mediated the association of BMI with clinical hand osteoarthritis (10.6 (6.2; 30.5)%) and structural knee osteoarthritis (3.1 (1.9; 7.3)%). Diastolic blood pressure (2.1 (1.6; 3.0)%) limitedly mediated the association between BMI and clinical knee osteoarthritis. PWV and popliteal VWT did not mediate the association between BMI and osteoarthritis.
Conclusion: Blood pressure and carotid IMT limitedly mediated the association of BMI with hand and knee osteoarthritis, suggesting that such mediation is questionable in the middle-aged population.
To cite this abstract in AMA style:
Loef M, van der Geest R, Lamb H, de Mutsert R, Rosendaal F, Kloppenburg M. Mediation of the Association Between Obesity and Osteoarthritis by Blood Pressure, Arterial Stiffness, and Subclinical Atherosclerosis [abstract]. Arthritis Rheumatol. 2020; 72 (suppl 10). https://acrabstracts.org/abstract/mediation-of-the-association-between-obesity-and-osteoarthritis-by-blood-pressure-arterial-stiffness-and-subclinical-atherosclerosis/. Accessed .« Back to ACR Convergence 2020
ACR Meeting Abstracts - https://acrabstracts.org/abstract/mediation-of-the-association-between-obesity-and-osteoarthritis-by-blood-pressure-arterial-stiffness-and-subclinical-atherosclerosis/