Session Information
Session Type: Poster Session A
Session Time: 10:30AM-12:30PM
Background/Purpose: Maternal smoking during pregnancy has been associated with a seemingly lower risk of juvenile idiopathic arthritis (JIA) in the child (1), contrasting with smoking’s established role as a risk factor for rheumatoid arthritis (RA) (2). Using large pregnancy and birth cohorts, we investigated the association between in-utero tobacco exposure and JIA and assessed the role of unmeasured confounding using a Mendelian Randomization (MR) framework.
Methods: We used three Scandinavian cohorts:1) The Norwegian Registry Linkage Cohort (NRC): All births in Norway from 2004-2020 (n >1 million children). 2) The Norwegian Mother, Father, and Child Cohort Study (MoBa): A pregnancy cohort from 1999-2009 (n >110 000 mother-infant pairs).3) The Danish National Birth Cohort (DNBC): A pregnancy cohort from 1996-2002 (n >90 000 mother-infant pairs). JIA cases were identified by ≥2 ICD-10 codes (M08/M09) by linking each cohort to national patient registries. Smoking was self-reported during pregnancy, and categorized as “none”, “1st trimester only”, and “beyond 1st trimester”. In MoBa, maternal genotyping data (n=41,887) enabled estimation of the association between maternal polygenic risk scores (PRS) for smoking initiation (3) and JIA in the child based on MR principles.Associations were estimated using logistic regression, adjusting for maternal education, parity, inflammatory rheumatic disease (MoBa and DNBC), region of birth (NRC and MoBa), and birth year. In the PRS-analyses, we only adjusted for the first 10 principal components. NRC and DNBC were meta-analyzed to increase precision, here excluding MoBa due to partial overlap with NRC (~220 JIA cases).
Results: 9.5% infants in the NRC, and 25% in both MoBa and DNBC, were exposed to in-utero tobacco exposure. We found no robust evidence that maternal smoking influenced JIA-risk in the child, with meta-analysis yielding an aOR of 1.07 (95% CI 0.84–1.37) for exposure only during the 1st trimester, and 1.15 (95% CI 0.95–1.39) for exposure beyond 1st trimester (Table 1; Figures 1 and 2). Maternal PRS for smoking initiation was strongly associated with self-reported smoking during pregnancy in MoBa (p< 0.001), supporting its validity as an instrument, but showed no associations with JIA (Table 1).
Conclusion: Across three prospective birth cohorts, using a triangulation approach, we find no evidence of a protective effect of maternal smoking during pregnancy on JIA risk, as previously reported. These findings underscore the importance of prospective designs and multiple approaches when investigating complex, confounding-prone exposures.References:1) Clarke SLN, et al. Rheumatology (Oxford). 2022;61(2) 2) Costenbader KH, et al. Am J Med. 2006;119(6)3) Liu M, et al. Nat Genet. 2019;51
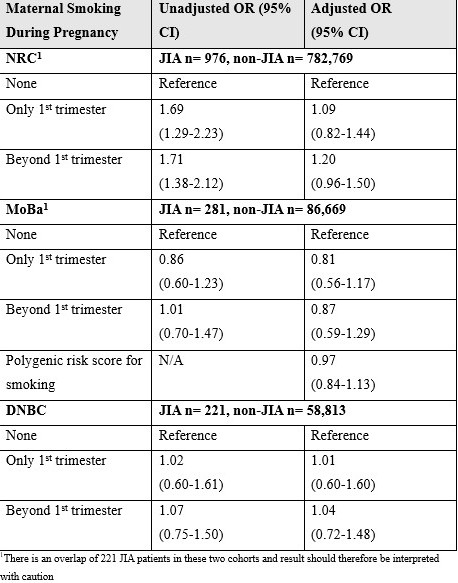 Table 1. Results of Analyses of Maternal Smoking Exposure and Child Risk of Developing JIA
Table 1. Results of Analyses of Maternal Smoking Exposure and Child Risk of Developing JIA
.jpg) Figure 1. Meta-analysis of NRC and DNBC: Associations between maternal smoking in 1st trimester and JIA (both sexes combined)
Figure 1. Meta-analysis of NRC and DNBC: Associations between maternal smoking in 1st trimester and JIA (both sexes combined)
.jpg) Figure 2. Meta-analysis of NRC and DNBC: Associations between maternal smoking beyond 1st trimester and JIA (both sexes combined)
Figure 2. Meta-analysis of NRC and DNBC: Associations between maternal smoking beyond 1st trimester and JIA (both sexes combined)
To cite this abstract in AMA style:
Dåstøl V, Haftorn K, Magnus M, Hestetun S, Håberg S, Rider L, Costenbader K, Caspersen I, Olsen S, Størdal K, Sanner H. Maternal Smoking During Pregnancy and Risk of Juvenile Idiopathic Arthritis (JIA): Triangulating Evidence from Polygenic Risk Scores and Meta-Analysis in Scandinavian Birth Cohorts [abstract]. Arthritis Rheumatol. 2025; 77 (suppl 9). https://acrabstracts.org/abstract/maternal-smoking-during-pregnancy-and-risk-of-juvenile-idiopathic-arthritis-jia-triangulating-evidence-from-polygenic-risk-scores-and-meta-analysis-in-scandinavian-birth-cohorts/. Accessed .« Back to ACR Convergence 2025
ACR Meeting Abstracts - https://acrabstracts.org/abstract/maternal-smoking-during-pregnancy-and-risk-of-juvenile-idiopathic-arthritis-jia-triangulating-evidence-from-polygenic-risk-scores-and-meta-analysis-in-scandinavian-birth-cohorts/
