Session Information
Session Type: Abstract Session
Session Time: 10:00AM-10:50AM
Background/Purpose: Inflammation and pain at entheseal sites are the key clinical signs in patients (pts) with axial spondyloarthritis (axSpA) and psoriatic arthritis (PsA).1 Magnetic resonance imaging (MRI) has been shown to be a sensitive tool to diagnose enthesitis in both bone and soft tissues, especially in cases of potential disconnect between pain and objective signs of inflammation at entheseal sites.2 ACHILLES (NCT02771210) is the largest prospective randomized controlled trial so far, investigating both clinical and imaging endpoints, with blinded and centrally read MRI data on heel enthesitis in pts with SpA.3 Here, we report MRI characteristics at screening in pts clinically diagnosed with heel enthesitis (N=204) from the ACHILLES trial.
Methods: ACHILLES included pts (≥18 years) with active PsA (CASPAR criteria and ≥1 tender joint count and swollen joint count) or axSpA (ASAS axSpA criteria with objective signs of inflammation at screening and/or hsCRP >5mg/L and total BASDAI ≥4), with clinical (presence of pain and tenderness) and STIR-MRI positive heel enthesitis, refractory to standard treatment (either NSAIDs or TNF-inhibitors). MRI-positive heel enthesitis was confirmed for all pts by local investigators and was defined as tendinitis and/or bone marrow edema (BME) in the insertional area of the Achilles’ tendon and/or the plantar aponeurosis. After randomization, all MRI were re-evaluated by two blinded central readers in a consensus read fashion for a priori defined qualitative and quantitative MRI parameters (based on PsAMRIS)4.
Results: According to central reading, 114/204 (55.9%) pts presented with MRI-positive heel enthesitis. The most frequently observed MRI feature was tendinitis, affecting 46.1% (94/204) of the population (Table 1). A total of 61 pts (29.9%) presented with BME affecting 1-33% of the heel (PsAMRIS category 1); out of these 40/61 (65.6%) had an edema length of ≤0.5 cm and 21/61 (34.4%) had an edema length of >0.5 cm. There was no bone erosion affecting more than 40% of the calcaneus; therefore, no erosions reported in the PsAMRIS categories 5 to 10 (Table 2). AxSpA pts presented with more severe edema compared to PsA pts (more pts having edema in category 2 or 3), resulting in a higher bone marrow edema score based on PsAMRIS categories and a higher composite score (Table 3).
Conclusion: Despite clinical assessment of enthesitis, only 56% of the ACHILLES patients presented with MRI-positive heel enthesitis according to central reading. These results indicate discrepancies in MRI evaluations between local and trained central readers. Furthermore, clinically assessed enthesitis might not necessarily correlate with imaging features of heel inflammation or chronic changes.
References:
- Schett, et al. Nat Rev Rheumatol. 2017;13(12):731-41.
- Poggenborg, et al. Ann Rheum Dis. 2015;74(5):823-9.
- Behrens, et al. Arthritis Rheumatol. 2019;71 (suppl 10). Abstract 2503.
- Bøyesen, et al. J Rheumatol. 2011;38;2034-2038.
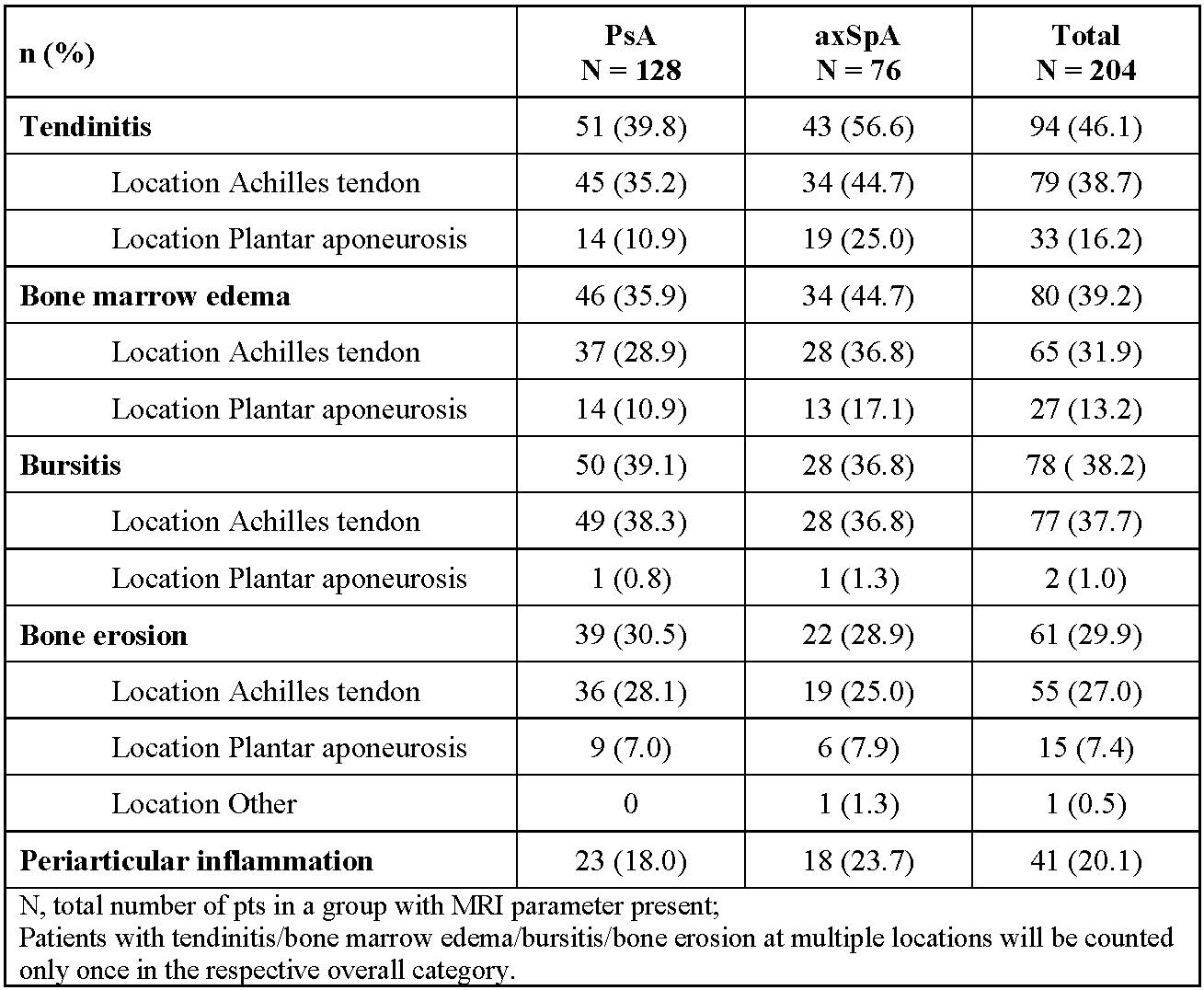 Table 1. MRI Parameter: Qualitative
Table 1. MRI Parameter: Qualitative
 Table 2. MRI Parameter: Quantitative
Table 2. MRI Parameter: Quantitative
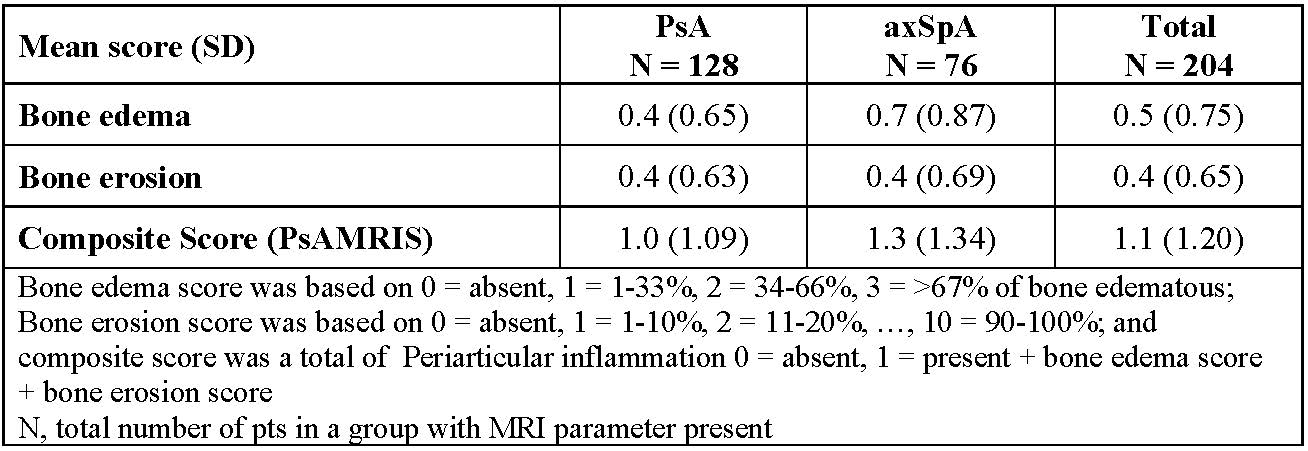 Table 3. MRI Parameter: Scores
Table 3. MRI Parameter: Scores
To cite this abstract in AMA style:
Baraliakos X, Sewerin P, De Miguel E, Kleinmond C, Shekhawat A, Jentzsch C, Wiedon A, Behrens F. Magnetic Resonance Imaging Characteristics in Patients with Spondyloarthritis and Clinical Diagnosis of Heel Enthesitis: Screening Data from a Phase 3 Trial [abstract]. Arthritis Rheumatol. 2020; 72 (suppl 10). https://acrabstracts.org/abstract/magnetic-resonance-imaging-characteristics-in-patients-with-spondyloarthritis-and-clinical-diagnosis-of-heel-enthesitis-screening-data-from-a-phase-3-trial/. Accessed .« Back to ACR Convergence 2020
ACR Meeting Abstracts - https://acrabstracts.org/abstract/magnetic-resonance-imaging-characteristics-in-patients-with-spondyloarthritis-and-clinical-diagnosis-of-heel-enthesitis-screening-data-from-a-phase-3-trial/
