Session Information
Session Type: Poster Session (Tuesday)
Session Time: 9:00AM-11:00AM
Background/Purpose: Osteoarthritis (OA) is a slowly progressing disease which may be asymptomatic for many years. Therapy development has been hampered by poor understanding of both structural progression and outcomes, largely based on imprecise radiographic assessment. A statistical shape model (SSM), a form of machine learning, identified a characteristic 3D OA bone shape from MR images, enabling investigation of the relationship between structure and clinical outcomes in the largest musculoskeletal MRI study to date.
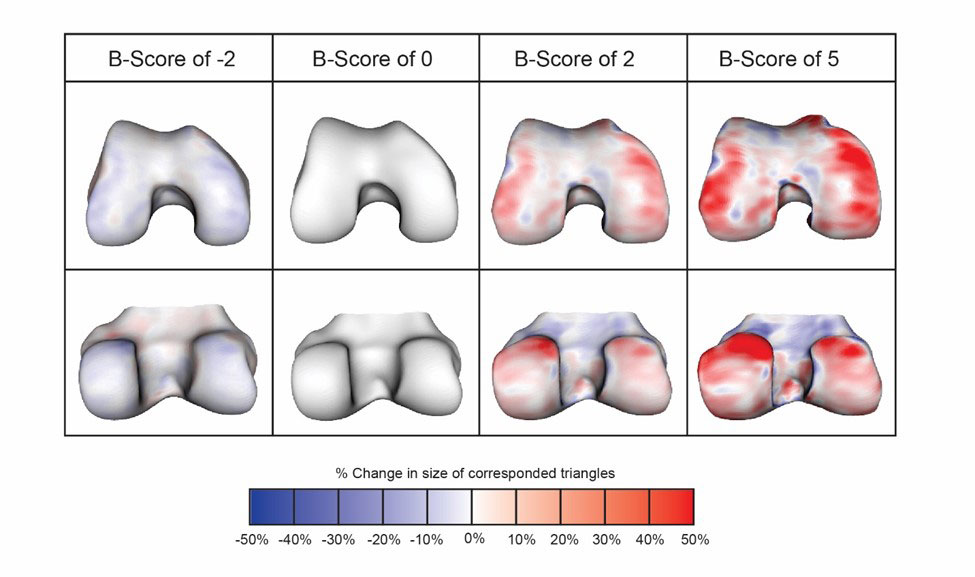
Methods: Construction of an SSM produces a “shape space,” spanned by principal components used to describe the training set of examples. Within this space, we constructed an “OA vector” passing through the mean shape of an “OA Group” (all knees KLG ≥2 at all 0, 1, 2, and 4 years), and the mean shape for a “Non-OA Group” (KLG = 0 at the same time points). Distances along the OA vector are normalized to a z-score (“B-score”), with the mean shape of the Non-OA Group for each sex represented as the OA vector origin; 1 unit represents 1 SD of the Non-OA Group along the OA vector (+ve values toward the OA Group). Each femur bone shape was projected orthogonally onto the OA vector to specify the corresponding B-score. Representative examples of the femur bone shape are shown in Fig. 1.
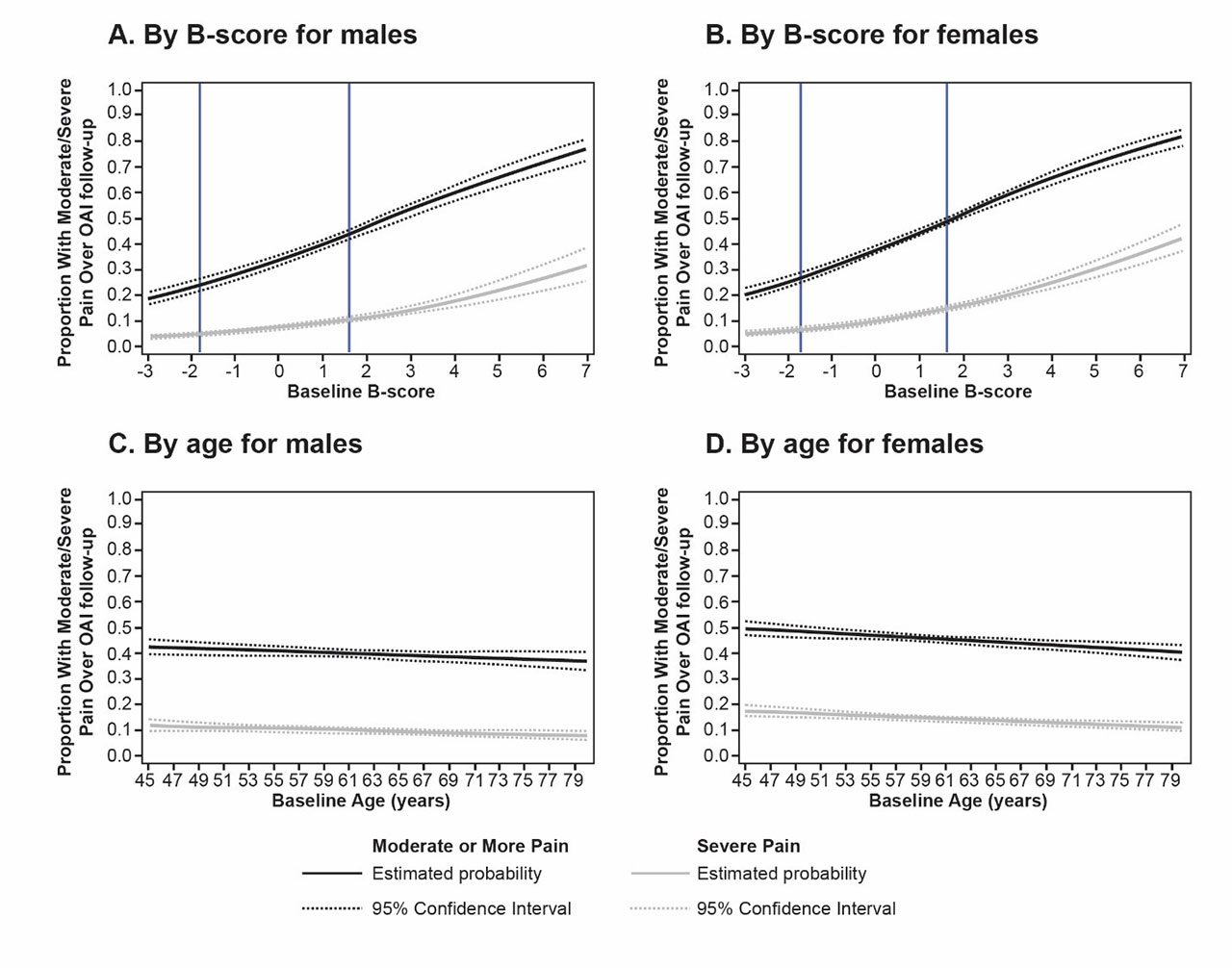
The B-score was automatically measured at multiple time points up to 8 years in the OAI (9,433 knees; 5,031 without OA; 47,858 MRI images). WOMAC-A (pain) on the 20-unit scale was dichotomized, first by presence of moderate or higher pain (score ≥4) and then again by presence of severe pain (score ≥8). Knee Replacement Surgery (KRS) was defined as having either total or partial knee arthroplasty within the follow-up period, adjudicated using post-surgery radiographs. Logistic regression analysis was performed modeling any reporting of pain or KRS at any single timepoint over the follow-up period for an individual knee by baseline B-score. This logistic regression was then repeated using baseline age.
Results: B-score was strongly associated with current and future pain; Fig. 2 displays the enhanced predictive power of B-score compared to age. Males and females were analyzed separately. However, an additional model combining both sexes was produced: for baseline B‑scores of 0 and 6 (incipient and advanced disease), future risk of painful knee within an average follow-up of 5 years was 36.0% (95% CI: 34.9 to 37.1) and 75.1% (72.6 to 77.5), respectively. Males had 210 KRS, females had 318. Although both baseline B-score and baseline age were both statistically significant at P< 0.001, Fig. 3 displays the enhanced predictive power of B-score compared to age for KRS. Using a combined model, future risk of KRS at B-scores of 0 and 6 was 2.3% (2.0 to 2.7) and 36.7% (32.5 to 41.1), respectively. Age had minimal utility in predicting pain or KRS.
Conclusion: By providing a continuous metric for OA, machine learning applied to a large dataset has for the first time demonstrated simple and strong relationships between bone shape and the current and future clinical outcomes. B-score provides accurate stratification for interventions and improved personalized assessment and is analogous to the T-score developed for osteoporosis.
To cite this abstract in AMA style:
Bowes M, Kacena K, Alabas O, Brett A, Dube B, Bodick N, Conaghan P. Machine Learning Defines the Relationship Between Structural Knee Osteoarthritis and Patient-Important Outcomes: An 8-year Study of 47,858 Knee MRIs from the Osteoarthritis Initiative (OAI) [abstract]. Arthritis Rheumatol. 2019; 71 (suppl 10). https://acrabstracts.org/abstract/machine-learning-defines-the-relationship-between-structural-knee-osteoarthritis-and-patient-important-outcomes-an-8-year-study-of-47858-knee-mris-from-the-osteoarthritis-initiative-oai/. Accessed .« Back to 2019 ACR/ARP Annual Meeting
ACR Meeting Abstracts - https://acrabstracts.org/abstract/machine-learning-defines-the-relationship-between-structural-knee-osteoarthritis-and-patient-important-outcomes-an-8-year-study-of-47858-knee-mris-from-the-osteoarthritis-initiative-oai/