Session Information
Date: Sunday, November 8, 2020
Title: SLE – Diagnosis, Manifestations, & Outcomes Poster II: Comorbidities
Session Type: Poster Session C
Session Time: 9:00AM-11:00AM
Background/Purpose: Systemic Lupus Erythematosus (SLE) a chronic inflammatory autoimmune disease that has the potential to affect every organ system. Studies have shown increased risk of certain malignancies among patients with SLE, with a potentially decreased risk of breast and prostate cancer related to anti-dsDNA antibodies (abs). This study examines the prevalence of malignancy types and relationships between clinical characteristics, autoantibody positivity and malignancy risk among patients with SLE.
Methods: Data was obtained from an ongoing longitudinal registry of patients with SLE (≥4 ACR classification criteria) and non-SLE population-matched controls. Information on demographics, medical and social history, and SLE characteristics (if applicable) was gathered from in-person interviews and medical record review. Disease damage was determined by SLICC/ACR Damage Index (SDI) with the malignancy item removed from scoring (“any damage present” if score ≥1). Children (age< 18 years) and those missing data on malignancy status were excluded from the study population. Analysis included descriptive statistics, Pearson’s chi-squared testing for categorical measures and two-sample t-tests for continuous measures.
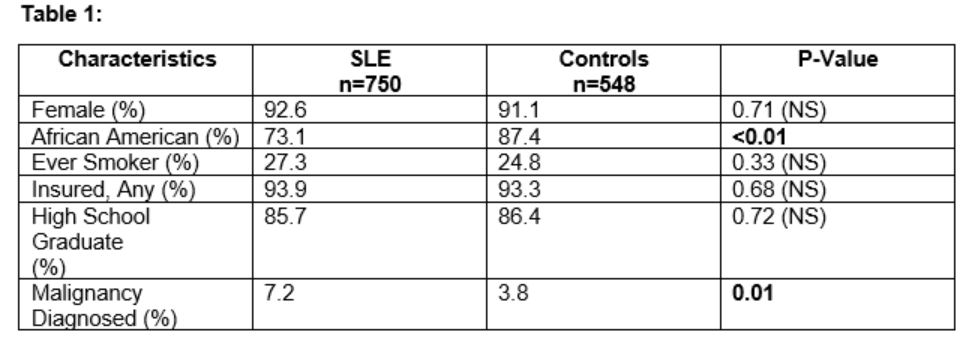
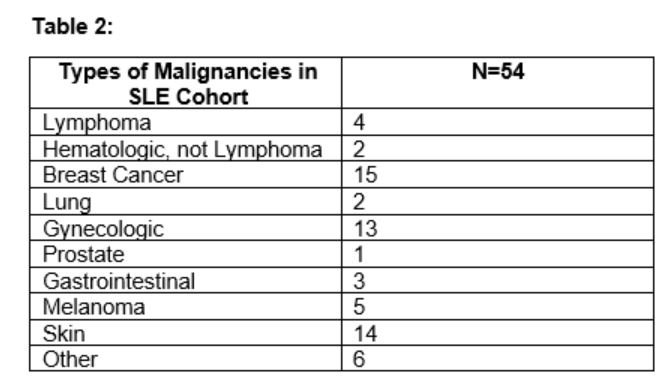
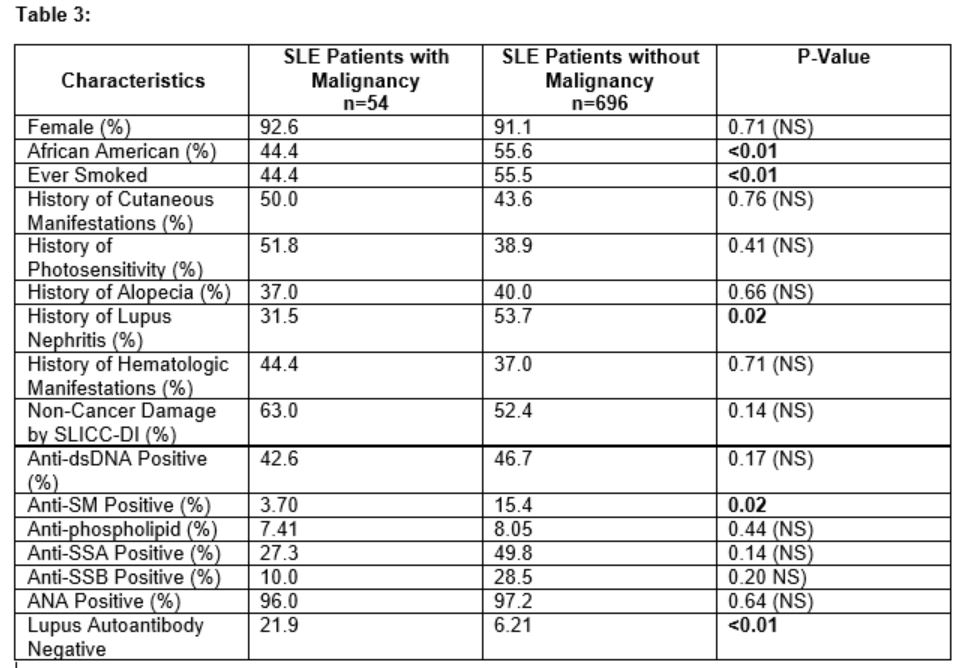
Results: A total of 750 SLE patients and 548 controls were included (Table 1). The mean age at SLE diagnosis was 31.1 years (SD ±13.8), mean age of malignancy diagnosis was 37.9 years (SD ±15.3), with mean age at last follow-up of 50.9 years (SD ±16.1). Comparing malignancy types between patients with SLE and controls, there was a higher incidence of gynecologic cancers (1.6% vs. 0.2%, p=0.01) and non-melanoma skin cancers (1.7% vs. 0.2%) among the patients. The 65 malignancies among the 54 patients with SLE are described in Table 2. The data did not show an association between BMI with either SLE or malignancy, but other clinical manifestations were associated with malignancy, as shown in Table 3. SLE patients that were lupus autoantibody negative (defined as being negative for dsDNA, SM, antiphospholipid, SSA and SSB antibodies), were statistically significantly more likely to have a malignancy history.
Conclusion: We found in this population of patients with SLE, that despite an overall increased risk of cancer, especially skin and gynecologic malignancies, compared to population-matched controls, the presence of certain SLE-associated autoantibodies decreased the likelihood of having a cancer history. These results support further studies to examine the relationship of autoantibodies, including anti-SM, anti-SSA and anti-SSB, and malignancy risk.
To cite this abstract in AMA style:
Huse S, Oates J, Gilkeson G, Kamen D. Lupus Antibodies in Relation to Malignancy [abstract]. Arthritis Rheumatol. 2020; 72 (suppl 10). https://acrabstracts.org/abstract/lupus-antibodies-in-relation-to-malignancy/. Accessed .« Back to ACR Convergence 2020
ACR Meeting Abstracts - https://acrabstracts.org/abstract/lupus-antibodies-in-relation-to-malignancy/