Session Information
Date: Monday, November 8, 2021
Session Type: Poster Session C
Session Time: 8:30AM-10:30AM
Background/Purpose: Advancing age, female sex and white race are well-known risk factors for development of giant cell arteritis (GCA). Recent studies suggest that certain metabolic features such as lower fasting blood glucose (FBG) may predispose to GCA. However, risk factors for development of GCA remain incompletely understood. We aimed to assess the frequency of comorbidities and metabolic risk factors at, and prior to, onset of GCA.
Methods: We conducted a retrospective case-control study of patients diagnosed with incident GCA in a geographically defined population from 01/01/2000 till 12/31/2019. Two age- and sex-matched controls were identified for every GCA case and assigned an index date corresponding to the incidence date of GCA. Twenty-five chronic conditions from either the Charlson, Elixhauser, or Rheumatic Disease Comorbidity Index were identified using ICD-9 diagnosis codes within a two-year lookback period; 2 or more codes ≥30 days apart were used to define a comorbidity. Prevalence of comorbidities, clinical and laboratory data among cases and controls were compared at incidence date and 5 years prior. Subjects with less than one year of diagnosis history were excluded from each analysis. Medical records of all subjects were manually abstracted for comorbidities and laboratory data at incidence date, at 5 years, and at 10 years prior to incidence date. Comparisons were performed using Chi square, Fisher exact, or t-tests.
Results: The cohort included 129 patients with GCA (74% female, mean age at diagnosis 77 years) and 253 controls (Table 1). At GCA incidence/index date, the prevalence of diabetes mellitus (DM) was lower in patients with GCA (5% vs 17%; p=0.001) while that of other comorbidities was similar in cases and controls. At 5 years prior to incidence/index date, cases had a lower prevalence of DM (2% vs 13%; p< 0.001) and hypertension (HTN) (27% vs 45%; p=0.002) as compared to controls. The mean number (SD) of comorbidities at 5 years prior to incidence/index date was lower [0.7 (1.0)] in cases than controls [1.3 (1.4)] (p< 0.001) (Table 1).
Moreover, at 5 years prior to incidence/index date, cases had a significantly lower median FBG (96 vs 104 mg/dL; p < 0.001) and body mass index (BMI) (25.8 vs 27.7 kg/m2; p-value=0.019) as compared to controls. At 10 years prior to the incidence/index date, the median FBG among cases was also lower (93 vs 98 mg/dL; p=0.002), although BMI was not significantly different at this time point. On the other hand, total cholesterol (median 211 vs 201 mg/dL; p=0.036), low-density lipoprotein (123 vs 112 mg/dL; p=0.043), and high-density lipoprotein (62 vs 57 mg/dL; p=0.032) were higher among cases compared with controls at 5 years prior to incidence/index date, and no different at 10 years prior. (Table 2).
Conclusion: Development of GCA was associated with a lower prevalence of DM and HTN, and lower total number of comorbidities, at 5 years prior to incidence date. FBG and BMI were also lower among individuals who later developed GCA, suggesting that metabolic factors influence the risk of GCA. Future studies to elucidate the patho-mechanisms underlying these observations are warranted.
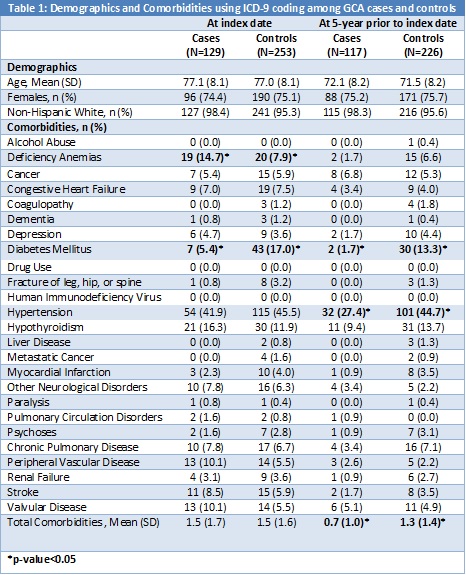 Table 1 Demographic and comorbidities using ICD-9 Coding among GCA cases and controls
Table 1 Demographic and comorbidities using ICD-9 Coding among GCA cases and controls
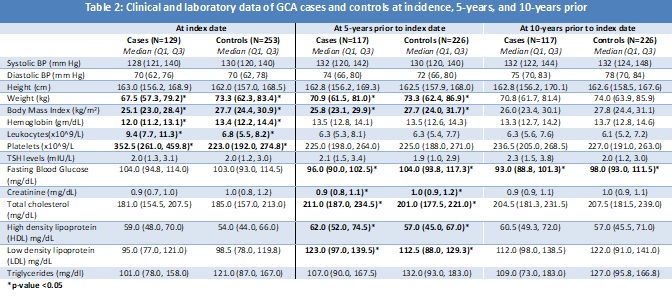 Table 2 Clinical and laboratory data of GCA cases and controls at incidence, 5-years and 10-years prior
Table 2 Clinical and laboratory data of GCA cases and controls at incidence, 5-years and 10-years prior
To cite this abstract in AMA style:
rakholiya j, Elfishawi M, Gunderson T, Crowson C, Matteson E, Turesson C, Wadström K, Weyand C, Koster M, Warrington K. Lower Frequency of Comorbidities Prior to Onset of Giant Cell Arteritis; A Population-based Study [abstract]. Arthritis Rheumatol. 2021; 73 (suppl 9). https://acrabstracts.org/abstract/lower-frequency-of-comorbidities-prior-to-onset-of-giant-cell-arteritis-a-population-based-study/. Accessed .« Back to ACR Convergence 2021
ACR Meeting Abstracts - https://acrabstracts.org/abstract/lower-frequency-of-comorbidities-prior-to-onset-of-giant-cell-arteritis-a-population-based-study/
