Session Information
Date: Monday, November 11, 2019
Title: Pediatric Rheumatology – ePoster II: SLE, Juvenile Dermatomyositis, & Scleroderma
Session Type: Poster Session (Monday)
Session Time: 9:00AM-11:00AM
Background/Purpose:
An estimated 10-20% of all patients with systemic lupus erythematosus (SLE) develop clinical disease before the age of 18 years and are therefore classified as juvenile-onset SLE (JSLE). JSLE patients have a higher prevalence of lupus nephritis (LN) compared to adult-onset SLE and decreased long-term survival compared to JSLE patients without LN. We aimed to identify clinical and laboratory predictors of LN in JSLE patients by comparing the baseline characteristics of JSLE patients with and without LN.
Methods:
This is a single-center retrospective study that included JSLE patients reviewed in our young adult and adolescent clinics after transitioning from paediatric services. All data was analysed descriptively. Mann-Whitney U or Chi-square test were performed to compare the characteristics between patients with and without LN. In addition, we performed uni and multivariate analysis to investigate potential predictor biomarkers for LN.
Results:
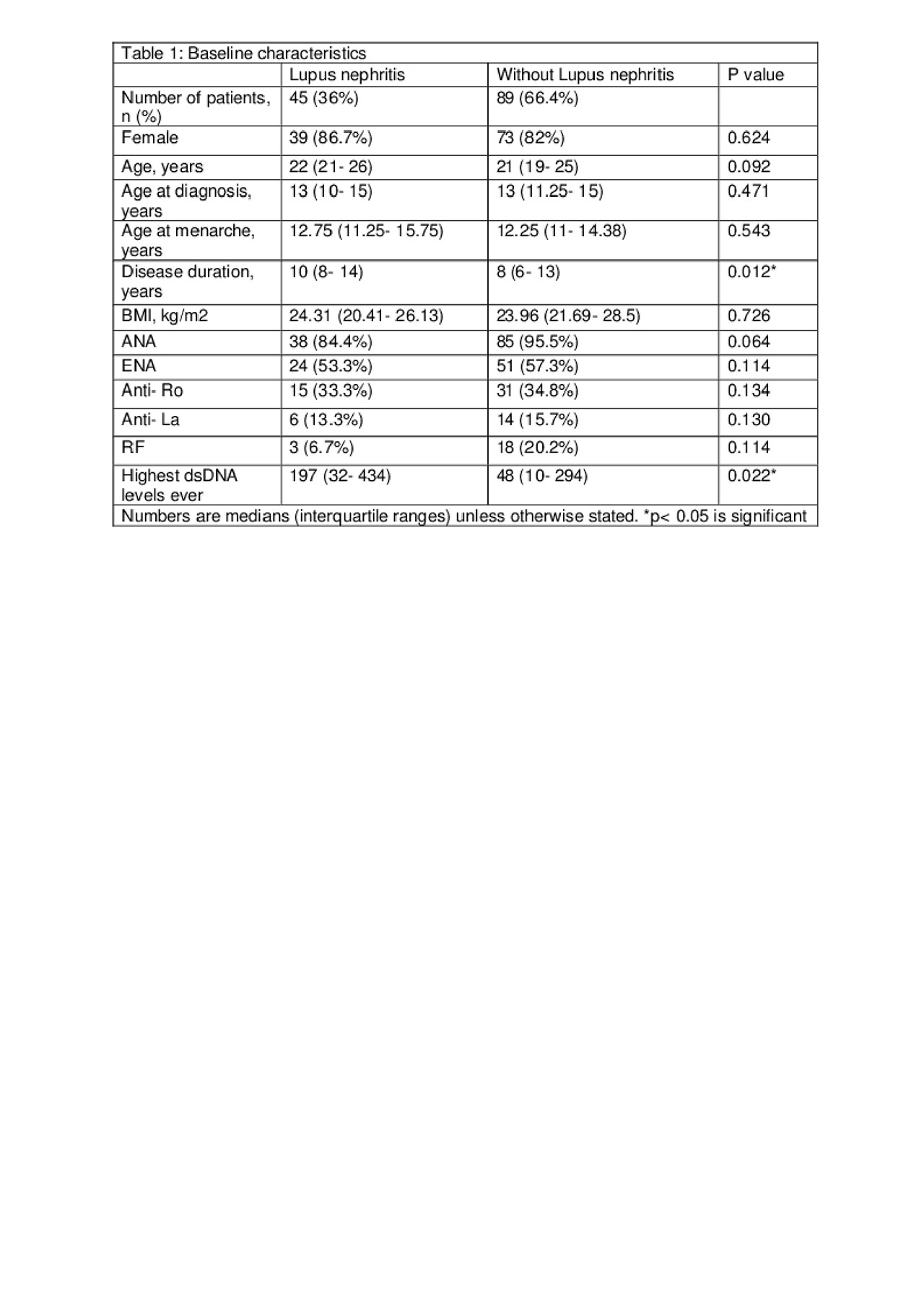
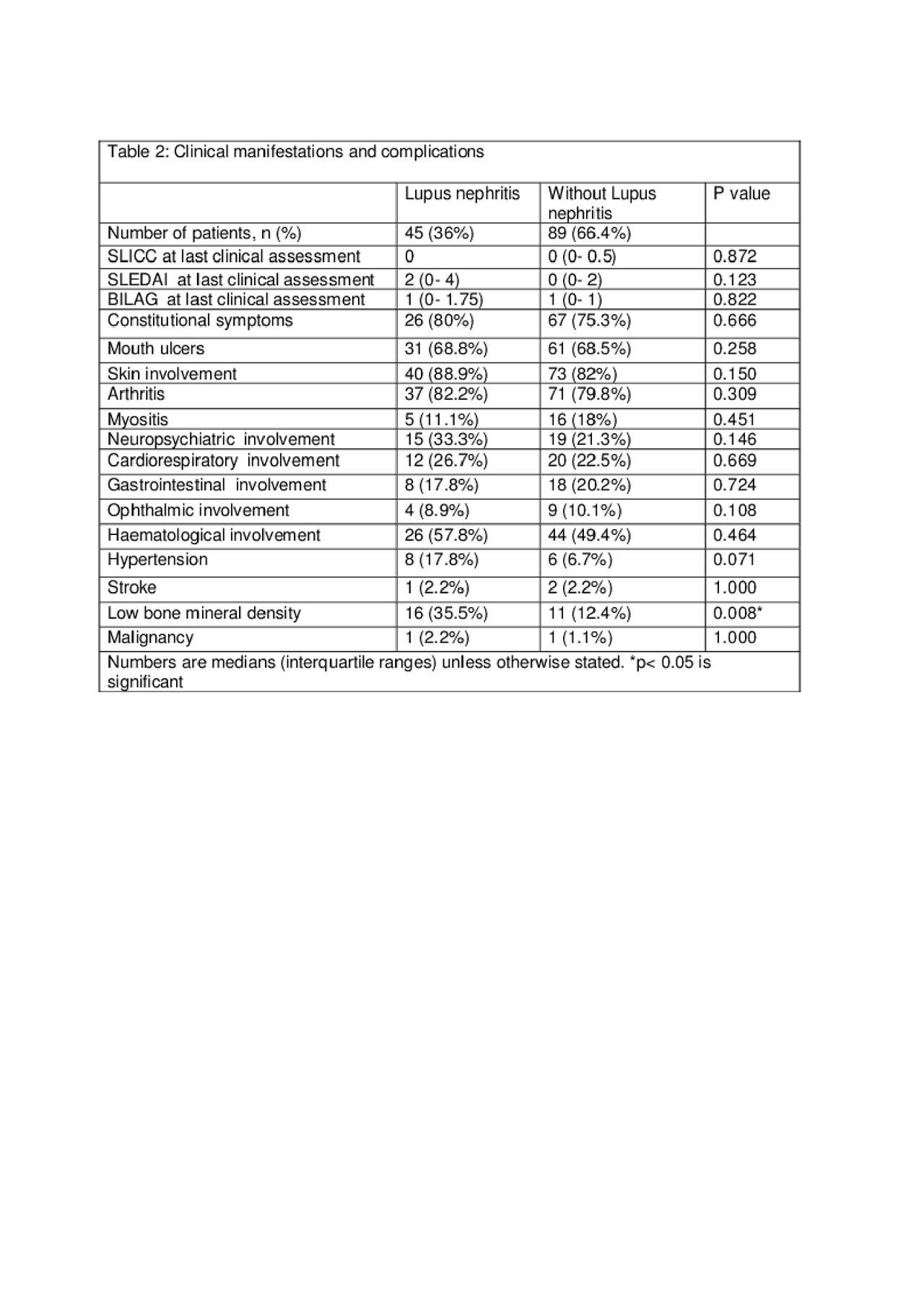
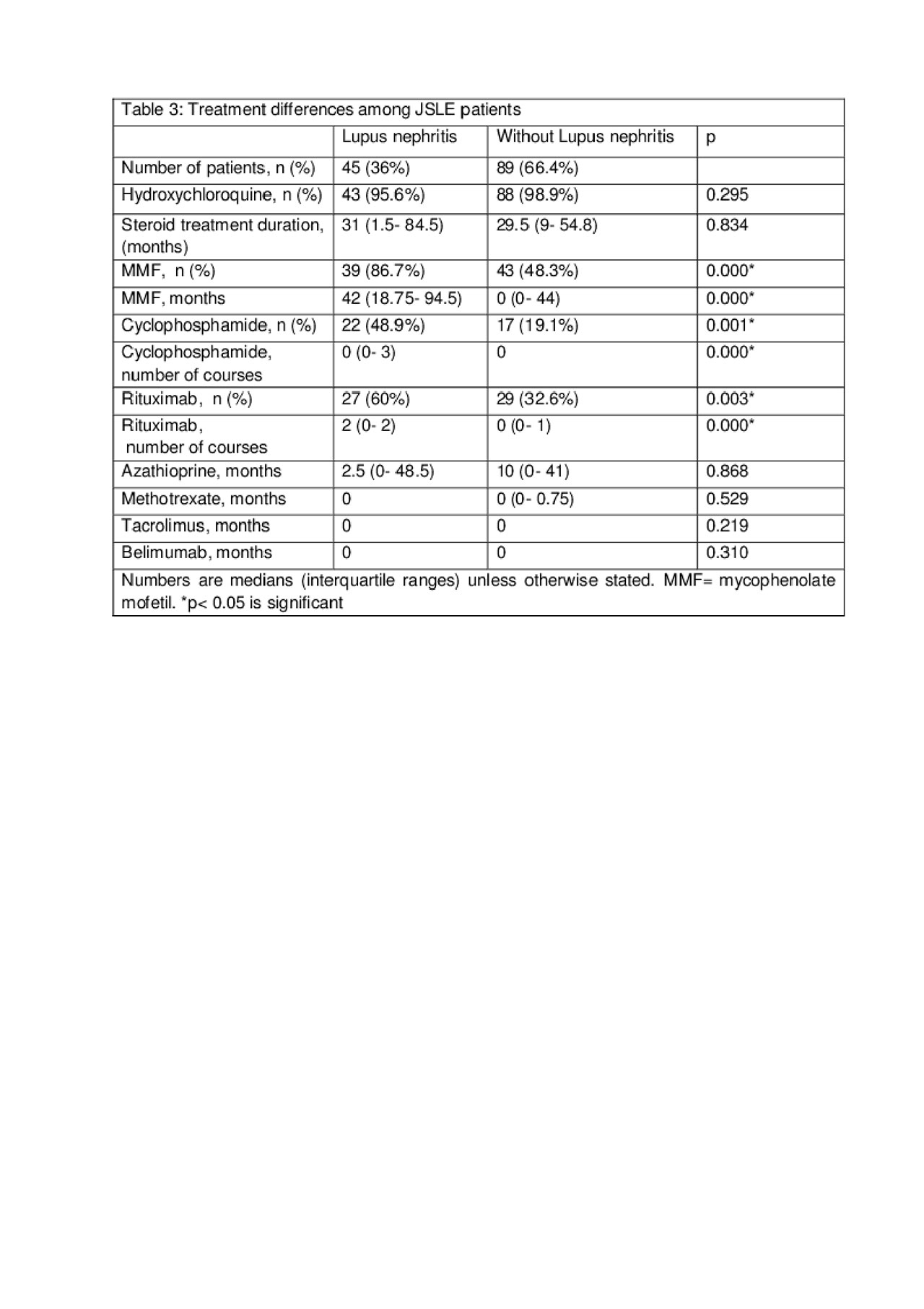
We identified 134 JSLE patients, 45 (34%) of which had LN. The baseline characteristics are detailed in table 1. As expected, the highest dsDNA levels ever were observed in patients with LN (p= 0.022).Patients with LN also had longer disease duration (p= 0.012). The overall clinical manifestations and complications did not differ between JSLE patients with or without LN, except for the prevalence of low bone mineral density (Table 2). Factors associated with low bone mineral density in a univariate logistic regression analysis were: the use of mycophenolate mofetil (p= 0.021) and the presence of LN (p= 0.007), while LN also associated with low bone density (p= 0.008) in a multivariate analysis. Skin involvement was the most common clinical manifestation in both JSLE patient groups. Treatment was more aggressive in patients with LN, including the use of cyclophosphamide, mycophenolate and rituximab, but there was no difference regarding the length of the steroid treatment (Table 3). The majority of patients (67%) had one flare of nephritis. For the remaining patients, the number of flares ranged from 2 (13%) to 12 (2.2%). The class of nephritis was reported in 34 out of 45 patients, and focal lupus nephritis (class III) was the most common type (44%) reported. There were no statistically significant differences in the baseline characteristics or treatments among the different classes of LN.
Conclusion: Low bone mineral density in patients with JSLE is well described. However, this is the first study highlighting the association of low bone density with LN independent of total duration of steroid treatment or other clinical manifestations.
To cite this abstract in AMA style:
Madenidou A, Mahfouz Y, Cheng O, El-Sharnouby F, Foley C, Ciurtin C. Low Bone Mineral Density Was Associated with Lupus Nephritis Irrespective of Duration on Steroid Treatment in a Large Observational Study of Juvenile Systemic Lupus Erythematosus Patients [abstract]. Arthritis Rheumatol. 2019; 71 (suppl 10). https://acrabstracts.org/abstract/low-bone-mineral-density-was-associated-with-lupus-nephritis-irrespective-of-duration-on-steroid-treatment-in-a-large-observational-study-of-juvenile-systemic-lupus-erythematosus-patients/. Accessed .« Back to 2019 ACR/ARP Annual Meeting
ACR Meeting Abstracts - https://acrabstracts.org/abstract/low-bone-mineral-density-was-associated-with-lupus-nephritis-irrespective-of-duration-on-steroid-treatment-in-a-large-observational-study-of-juvenile-systemic-lupus-erythematosus-patients/