Session Information
Session Type: Poster Session C
Session Time: 9:00AM-11:00AM
Background/Purpose: MRI has identified joint tissues affected during knee OA development, though the relative importance of structures in the pathogenic process is unknown. Our objective was to estimate relative contributions of structural abnormalities to risk of incident radiographic knee OA (iRKOA), with assessment of longitudinal MRI during 10 year follow-up.
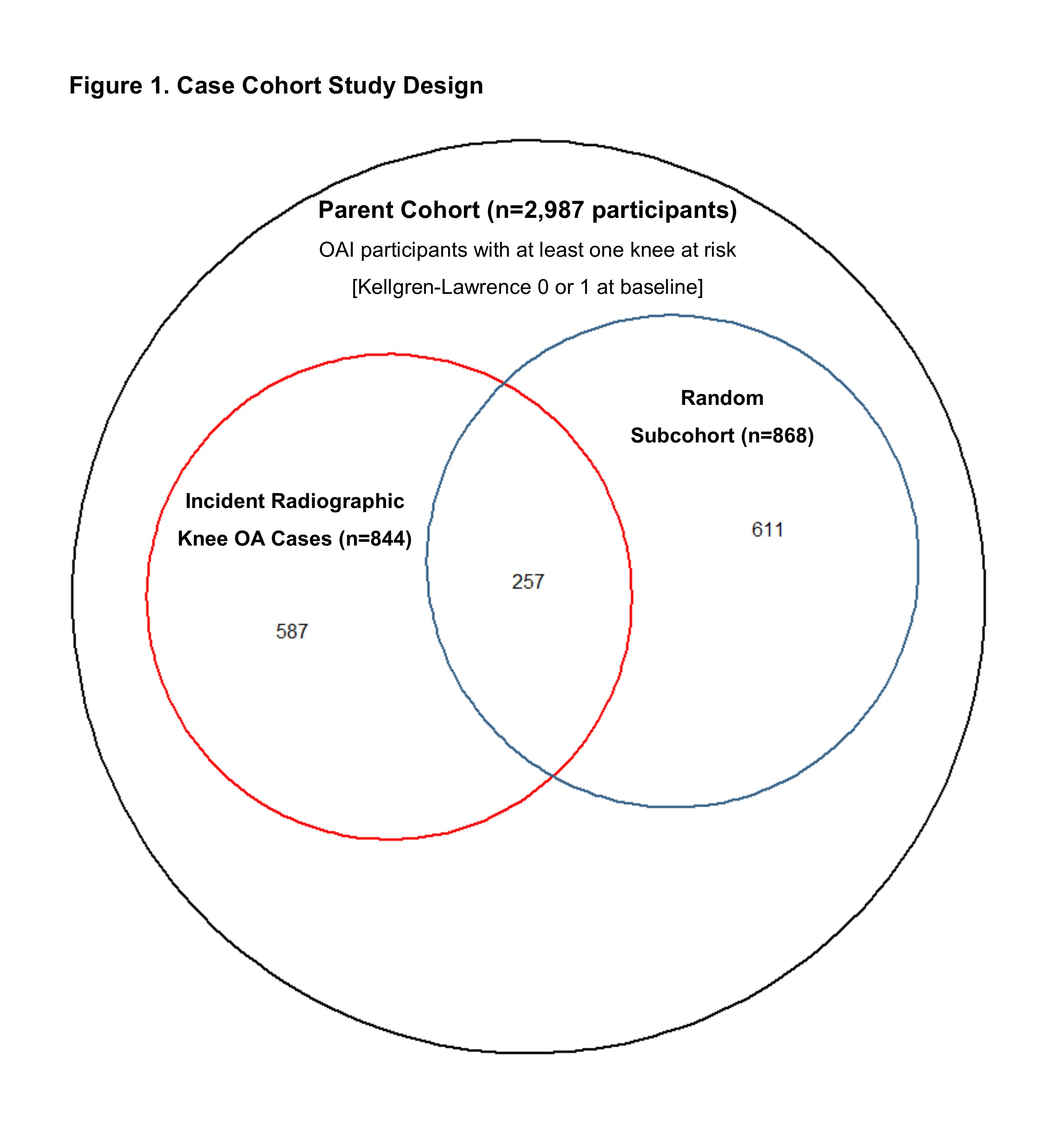
Methods: We conducted a case-cohort study with 10 year follow-up. The parent cohort included 2,987 Osteoarthritis Initiative participants with at least one knee at risk of developing iRKOA (i.e., Kellgren-Lawrence [KL] 0 or 1 at baseline). Within the parent cohort, participants who developed iRKOA (cases, n=844) and a random sample of the parent cohort (subcohort, n=868) were identified for MRI readings, a total of 1,455 participants (Figure 1). If a participant had two knees at risk, we selected the first knee to develop iRKOA or otherwise selected a knee at random (one knee per person).
Participants underwent bilateral posteroanterior fixed-flexion weight-bearing x-ray at baseline and annually through year 4, and then every two years until year 10; x-rays were centrally read for KL grade. 3T MRI was acquired at clinic visits up to year 8; longitudinal structural abnormalities in knees identified as cases and/or in the subcohort were graded using the MRI Osteoarthritis Knee Score (MOAKS).
We fit Cox models for time to iRKOA, with subcohort controls weighted inversely proportional to the sampling fraction; longitudinal structural features were included as time-varying predictors, lagged from the visit prior to each x-ray to establish temporality. We fit feature-specific models for bone marrow lesions (BML), cartilage damage, and meniscal damage with maximum scores in each compartment (i.e., medial tibiofemoral [TF], lateral TF, patellofemoral [PF]), as well as an inflammation model for whole-knee effusion-synovitis (ES) and Hoffa-synovitis (HS). We also fit a full model with all features.
Results: Time to iRKOA is shown in Figure 2. The subcohort reflected the parent cohort, with a mean age of 60 years (SD 9), 55% female, 84% white and 14% African American, and predominately overweight (40%) or obese (32%).
In feature-specific models, all structural abnormalities were associated with iRKOA, and in nearly every compartment. The magnitude of association for specific abnormalities attenuated in the full model that included all features, though medium/large ES and PF cartilage damage of >10% surface area with >10% full-thickness or >75% surface area was associated with at least a two-fold increase in risk of iRKOA (based on lower bounds of the 95%CIs). Small ES, large medial TF BMLs, and PFJ cartilage damage of 10-75% surface area with any full-thickness, and lateral meniscus maceration were estimated to increase risk by at least 50% (Table 1).
Conclusion: While all structural abnormalities were associated with iRKOA in at least one compartment, our findings suggest that ES, PF cartilage damage, large medial TF BMLs, and lateral meniscus maceration are particularly indicative of increased risk of iRKOA. Varied structural abnormalities associated with knee OA development suggests heterogenous disease pathology that may require custom multifaceted treatment approaches.
To cite this abstract in AMA style:
Kwoh C, Guermazi A, Ashbeck E, Hu C, Bedrick E, Sharma L, Eaton C, Hochberg M, Jackson R, McAlindon T, Nevitt M, Cauley J, Roemer F. Longitudinally Assessed Structural Abnormalities on MRI and Relative Contributions to Risk of Incident Radiographic Knee Osteoarthritis over 10 Years of Follow-up [abstract]. Arthritis Rheumatol. 2020; 72 (suppl 10). https://acrabstracts.org/abstract/longitudinally-assessed-structural-abnormalities-on-mri-and-relative-contributions-to-risk-of-incident-radiographic-knee-osteoarthritis-over-10-years-of-follow-up/. Accessed .« Back to ACR Convergence 2020
ACR Meeting Abstracts - https://acrabstracts.org/abstract/longitudinally-assessed-structural-abnormalities-on-mri-and-relative-contributions-to-risk-of-incident-radiographic-knee-osteoarthritis-over-10-years-of-follow-up/