Session Information
Date: Tuesday, November 14, 2023
Title: (2370–2386) Vasculitis – ANCA-Associated Poster III: Biomarkers & Renal Outcomes
Session Type: Poster Session C
Session Time: 9:00AM-11:00AM
Background/Purpose: ANCA-associated vasculitis (AAV) commonly causes renal damage, leading to a spectrum of chronic kidney disease (CKD) and end-stage renal disease (ESRD). Quantitative descriptions of the longitudinal course of renal dysfunction in AAV have recently been published from the 2002-2017 Mass General Brigham (MGB) AAV cohort. We aimed to further investigate these findings in an expanded cohort with additional years of follow-up.
Methods: We included patients from the MGB AAV cohort (2002-2022). A “baseline” measurement (±30 d from treatment initiation, the index date) of renal function was required along with one additional test. Renal function was assessed at up to monthly intervals, from -12 m to +24 m relative to the index date. Group-based trajectory modeling was used to identify distinct renal function trajectories. We assessed between-group differences (between all trajectory groups) with the chi-square and Kruskall-Wallis tests. Time to ESRD was compared using the log-rank test.
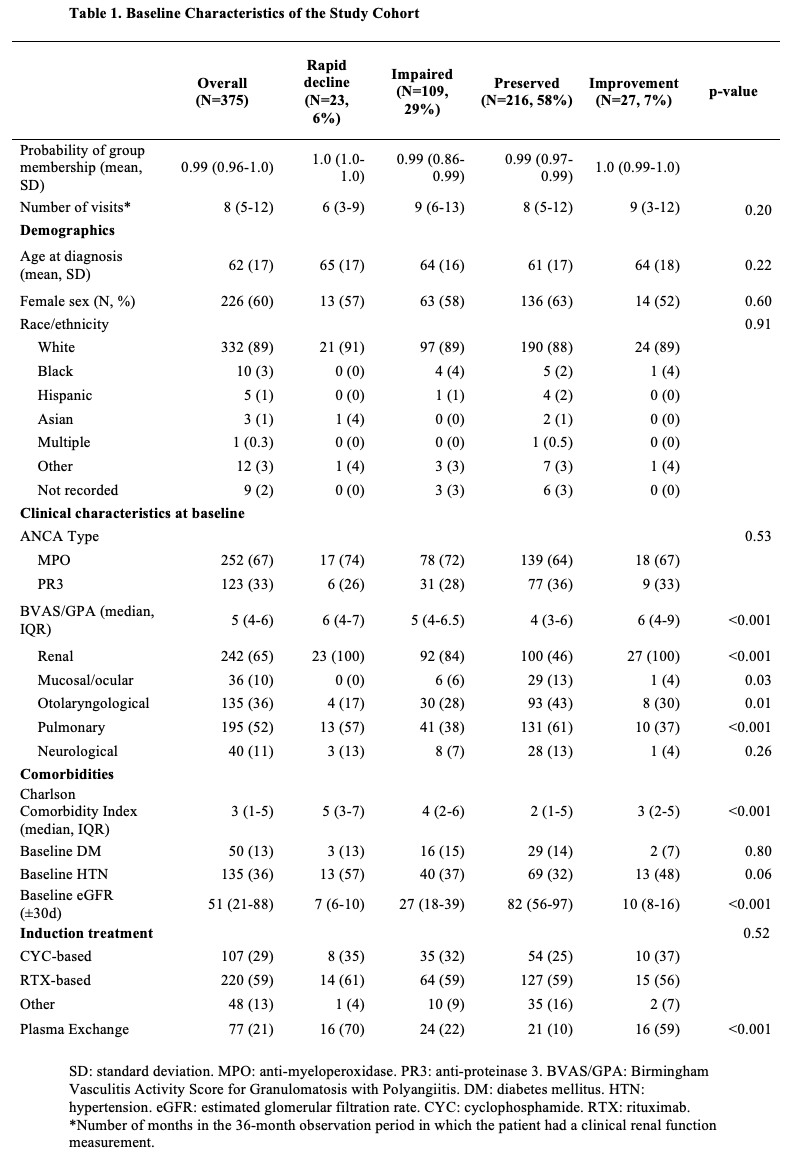
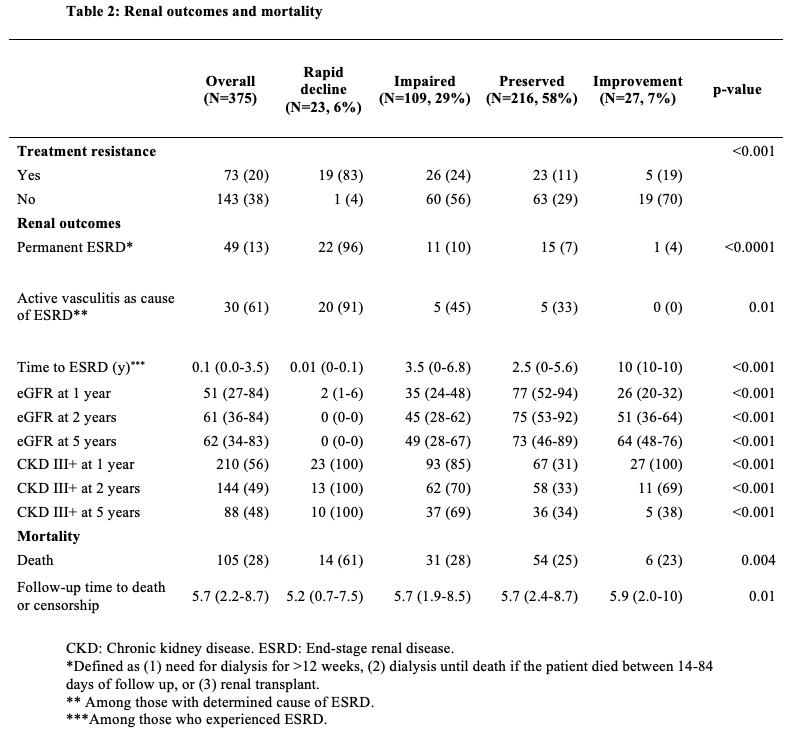
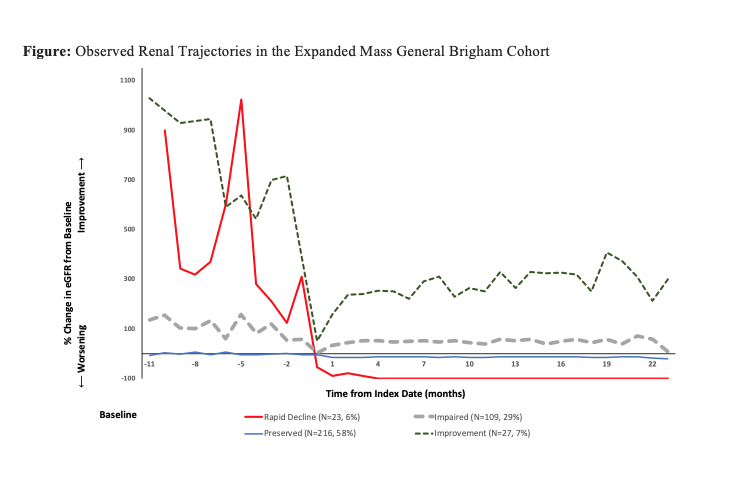
Results: We identified 4 renal trajectory groups among 375 patients: rapid decline (N=23 [6%]), impaired (N=109 [29%]), preserved (N=216 [58%]), and improvement (N=27 [7%]) (Figure). The median posterior probability of group membership was >0.98 in all groups, indicating excellent fit. Age, sex, race and ANCA type were not statistically different between groups. Renal vasculitis was found in all patients in the rapid decline (N=23 [100%]) and improvement (N=27 [100%]) groups, and in a majority of the impaired (N=92 [84%]), compared to a minority of the preserved group (N=100 [46%]; p< 0.001). Pulmonary vasculitis was more common among the rapid decline (N=13 [57%]) and preserved (N=131 [61%]) groups, compared to the impaired (N=41 [38%]) and improvement (N=10 [37%]) groups (p< 0.001). Otolaryngological and mucosal manifestations were most common in the preserved group (Table 1). The rapid decline group had the greatest baseline comorbidity, followed by the impaired group (p< 0.001; Table 1). Diabetes was equally common between groups, but there was a strong trend toward a higher rate of hypertension among the rapid decline and improvement groups vs the impaired and preserved groups (p=0.06). Disease activity by baseline Birmingham Vasculitis Activity Score was higher in the rapid decline (6 [4, 7]) and improvement (6 [4, 9]) groups, compared to the impaired (5 [4, 6.5]) and preserved (4 [3, 6]) groups (p< 0.001). ESRD occurred in 49 patients. In the rapid decline group, 22 patients (96%) experienced ESRD, compared to 11 (10%) in impaired, 15 (7%) in preserved and 1 (4%) in the improvement group (Table 2). ESRD occurred at a median of < 1 m from the index date in rapid decline vs 3.5 y (IQR 0, 6.8) in impaired and 2.5 y (IQR 0, 5.6) in the preserved group (log-rank p< 0.001). The cause of ESRD was active AAV in 91% of cases in the rapid decline, vs 45% in the impaired and 33% in the preserved group (p=0.01; Table 2).
Conclusion: We identified 4 distinct renal trajectory groups in an expanded AAV cohort. Trajectory groups were distinguished by variation in baseline comorbidity, rates of ESRD and CKD, and timing and cause of ESRD. Confirmation in a separate cohort will be required.
To cite this abstract in AMA style:
Hanberg J, Cook C, Fu X, Choi H, Zhang Y, Wallace Z. Longitudinal Trajectories of Renal Function in ANCA-Associated Vasculitis: Findings from the Expanded Mass General Brigham Cohort [abstract]. Arthritis Rheumatol. 2023; 75 (suppl 9). https://acrabstracts.org/abstract/longitudinal-trajectories-of-renal-function-in-anca-associated-vasculitis-findings-from-the-expanded-mass-general-brigham-cohort/. Accessed .« Back to ACR Convergence 2023
ACR Meeting Abstracts - https://acrabstracts.org/abstract/longitudinal-trajectories-of-renal-function-in-anca-associated-vasculitis-findings-from-the-expanded-mass-general-brigham-cohort/