Session Information
Session Type: Poster Session A
Session Time: 9:00AM-11:00AM
Background/Purpose: In SLE, periods of relative quiescence are punctuated by flares in disease activity that can lead to extensive tissue damage and morbidity. Existing studies suggest that flare onset is linked to immune cell subsets involved in ANA production, including activated memory T helper cells, plasma cells, and age-associated B cells (ABCs); however, it is largely unknown how these and other immune subsets differ between flare and inactive disease, particularly in the period post-flare.
Methods: Healthy controls (HC, n=16) and acute flare (n=47) or inactive (n=25) SLE patients were recruited, with patients diagnosed based on the 1997 ACR criteria. Flare patients were within 1 month of flare onset (a clinical SLEDAI-2K >0 requiring a change in therapy) while inactive patients had to be inactive for ≥1 year (clinical SLEDAI-2K=0) and on ≤10mg prednisone at recruitment. All patients had blood collected at first visit as well as at 6M and 12M follow-ups. Freshly isolated PBMCs were stained with various fluorochrome-conjugated antibodies to identify immune cell populations by flow cytometry. Statistical significance was determined using Mann-Whitney U tests to compare baseline groups and Wilcoxon matched-pairs signed rank tests to compare baseline and follow-up visits.
Results: SLE patients differed significantly from HC in multiple immune cell subsets at baseline, with higher proportions of ABCs, T peripheral helper (Tph) cells, regulatory T (Treg) cells, and pro-inflammatory monocytes, as well as a trend to higher plasmablasts (see Table 1). However, stratification of SLE patients into acute flare and inactive groups revealed limited differences between these groups at baseline. While flare patients had significantly higher proportions of ABCs as well as significantly lower proportions of NK cells, pDCs and mDCs as compared to inactive patients, the majority of monocyte, B, T, and antibody-producing cell subsets did not differ between flaring and inactive patients, suggesting that these populations are not enriched in the blood during flare. In contrast, flare patients diverged significantly from inactive patients in multiple immune subsets at 6M and/or 12M following flare treatment, showing significant increases in B cell activation (p=0.0118), CD16+ monocytes (p< 0.0001), transitional B cells (p=0.0006), Tregs (p=0.0093), Tph cells (p=0.0385) and Tph17 cells (p=0.0055). These differences appeared to stem from increases in these populations in flare patients during the post-flare period, while inactive patients remained relatively stable over the same time frame (see Figures 1 and 2 for representative results).
Conclusion: Our results suggest that at the time of acute flare many of the activated immune cell populations that are proposed to participate in flare are absent from the peripheral blood. Instead, differences between flaring and inactive patients become more apparent in the months following flare treatment, as activated immune cells are not recruited into and/or migrate out of inflamed tissues. These findings highlight the importance of longitudinal studies of flare in SLE.
 Table 1. There are significant differences between healthy controls and lupus patients in multiple immune cell subsets at baseline; however, many of these populations do not show further differences between flare and inactive patients.
Table 1. There are significant differences between healthy controls and lupus patients in multiple immune cell subsets at baseline; however, many of these populations do not show further differences between flare and inactive patients.
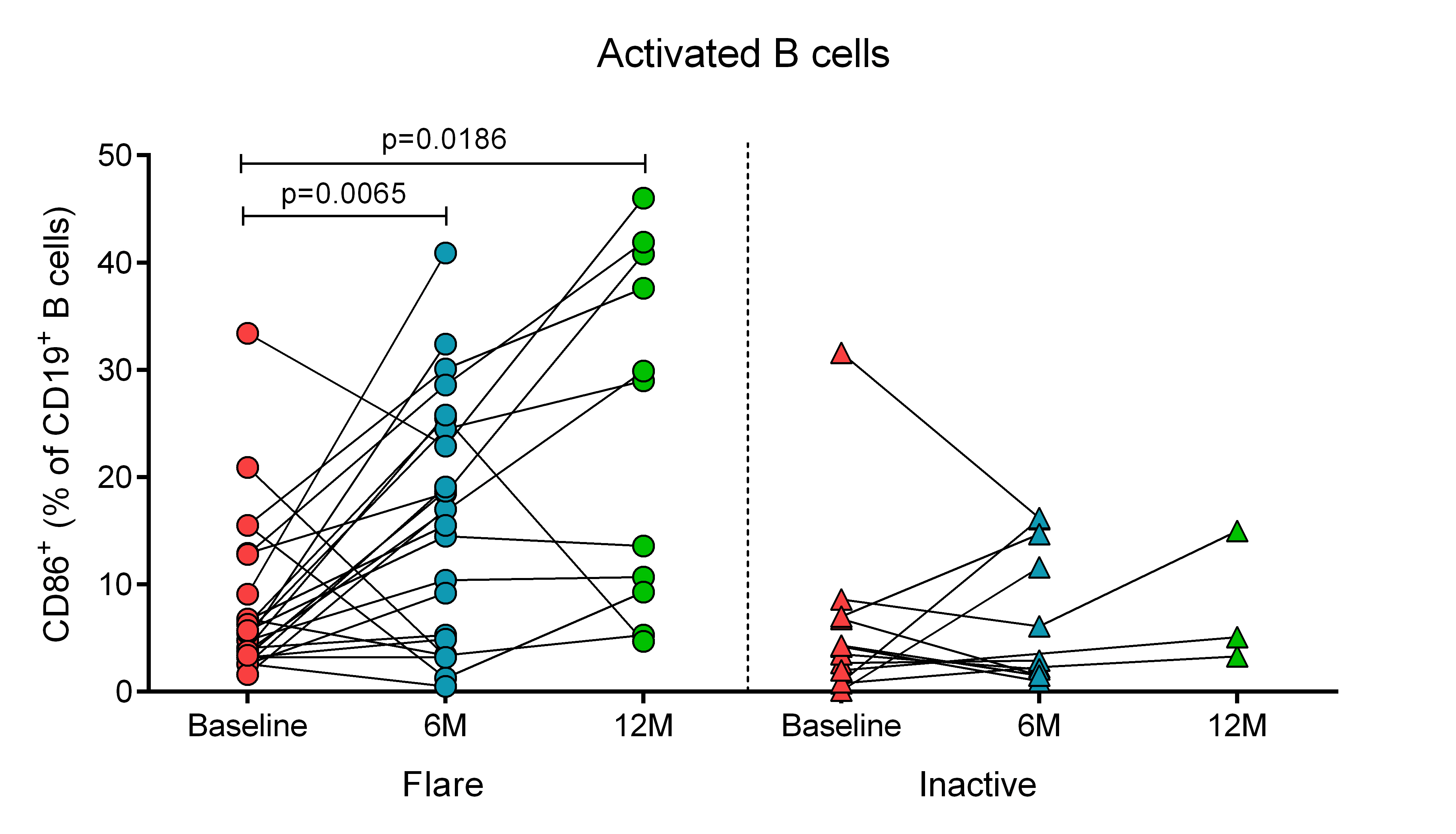 Figure 1. Flare patients show significant increases in the proportions of activated B cells in the blood at 6M and 12M post-flare, while levels remain stable in inactive patients over time.
Figure 1. Flare patients show significant increases in the proportions of activated B cells in the blood at 6M and 12M post-flare, while levels remain stable in inactive patients over time.
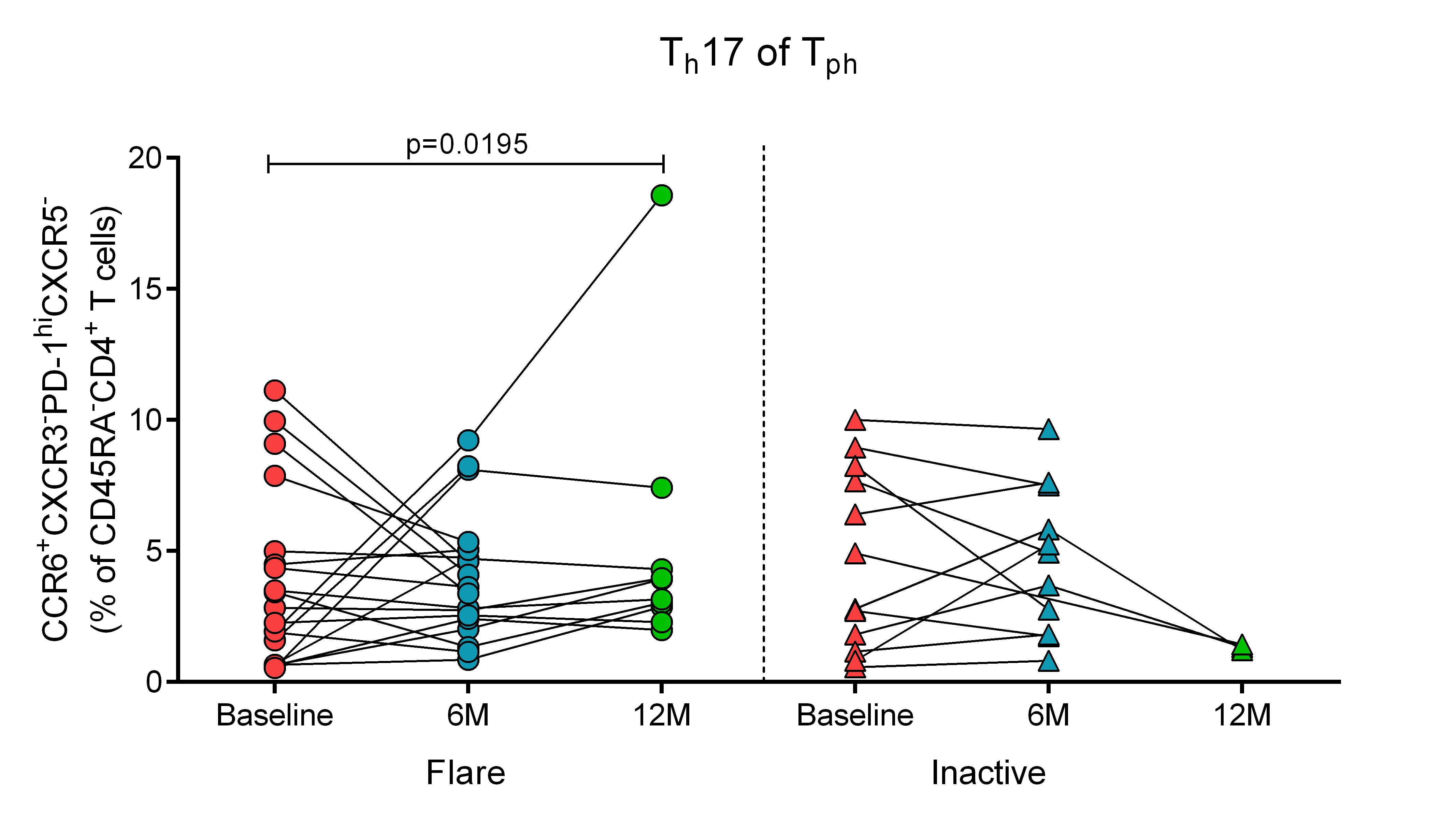 Figure 2. Flare patients show significant increases in the proportions of Tph Th17 cells in the blood at 12M post-flare, while levels remain stable in inactive patients over time.
Figure 2. Flare patients show significant increases in the proportions of Tph Th17 cells in the blood at 12M post-flare, while levels remain stable in inactive patients over time.
To cite this abstract in AMA style:
Manion K, Bonilla D, Gladman D, Urowitz M, Touma Z, Wither J. Longitudinal Study of Acute SLE Flare Reveals Dynamic Changes in Multiple Immune Cell Subsets [abstract]. Arthritis Rheumatol. 2020; 72 (suppl 10). https://acrabstracts.org/abstract/longitudinal-study-of-acute-sle-flare-reveals-dynamic-changes-in-multiple-immune-cell-subsets/. Accessed .« Back to ACR Convergence 2020
ACR Meeting Abstracts - https://acrabstracts.org/abstract/longitudinal-study-of-acute-sle-flare-reveals-dynamic-changes-in-multiple-immune-cell-subsets/
