Session Information
Session Type: Abstract Session
Session Time: 2:15PM-2:30PM
Background/Purpose: Non-steroidal anti-inflammatory drugs (NSAIDs) are a primary treatment for osteoarthritis (OA). It is uncertain, however, whether regular use of NSAIDs affects the risk of structural progression and ultimately increase joint replacement risk. Reports suggest that users of analgesics including NSAIDs may experience more progressive structural deterioration than non-users. On the other hand, NSAIDs may reduce intra-articular inflammation sufficiently to minimize potential damage. Whereas regular use of prescription NSAIDs is common in persons with OA, the long-term effects of pain-relieving interventions on structural damage are not fully characterized. Previous studies focused on short-term effects and only compared always-users of NSAIDs with non-users and had limited ability to mitigate confounding by indication. We used a causal inference-based approach, and designed a hypothetical longitudinal trial from observational data to assess the risk of a knee replacement (KR) under various time-varying regimens of regular prescription NSAIDs use.
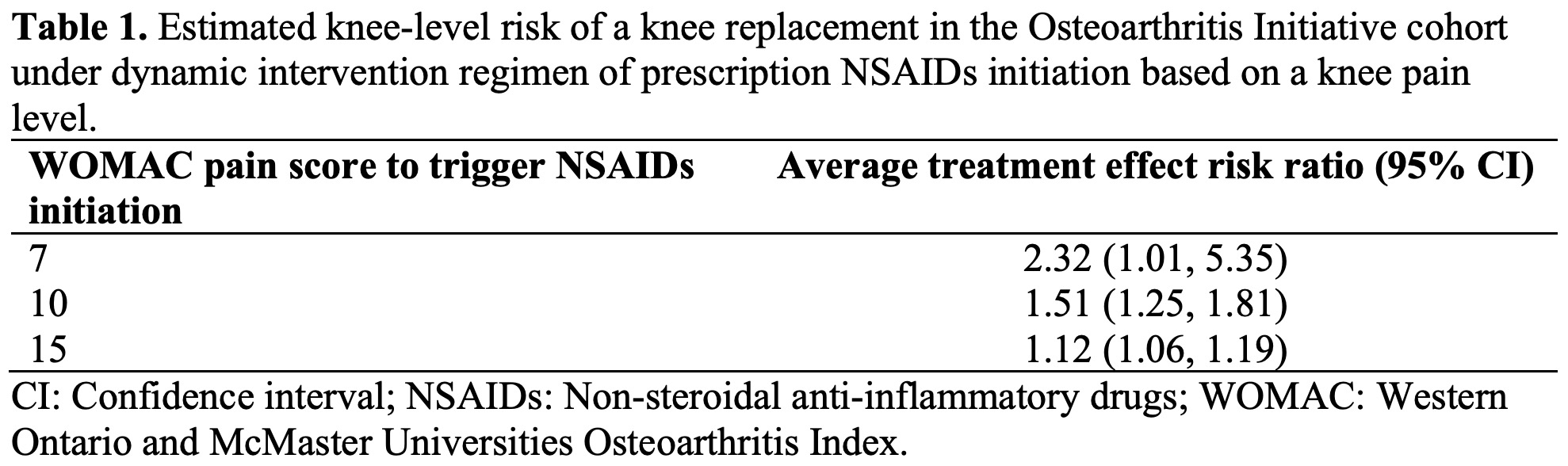
Methods: We included 8 years of data from the Osteoarthritis Initiative (OAI) cohort, including baseline, 12-, 24-, 36-, 48-, 72-, and 96-month OAI study visits. Study outcome was defined as a KR. Study exposure was defined as the regular use of any prescription NSAIDs, which was determined at every study visit. Study covariates included baseline and time-dependent confounders measured at all OAI visits that included knee pain characterized by the Western Ontario and McMaster Universities Osteoarthritis Index (WOMAC) pain subscale. We used targeted learning, a double-robust causal inference-based methodology, to compare the risk of a knee replacement under hypothetical intervention regimens that included comparing no NSAID use in persons with painful knees to a hypothetical regimen of regular NSAIDs use in the same persons and under the same conditions. We examined KR risk for hypothesized NSAIDs initiation at knee pain levels of 7, 10, and 15 on the 0-20 WOMAC scale, compared to no NSAID use at the same pain levels.
Results: Data included 528 KR events (in 9592 knees; 5.5%) in 4796 persons (58.5% female; baseline mean age = 61.2 [SD = 9.2]). The estimated reference risk of a KR event in OAI (i.e., the risk for the no intervention regimen), adjusted for loss to follow-up and death, was 5.9% (95% CI: 5.2%, 6.5%). KR risk increased by 232%, 51%, and 12% when NSAIDs initiation was triggered at WOMAC pain level of 7, 10, and 15, respectively, suggesting an increased risk of KR with NSAID use especially when prescription NSAIDs were initiated at lower knee pain levels. Examining WOMAC pain < 7 was not possible given the rarity of regular NSAID use at this threshold in OAI participants. To adjust for pain severity, we used WOMAC pain score at the annual exam prior to report of regular NSAID use and if pain worsened over the year, triggering NSAID use, our findings may overestimate NSAID risk.
Conclusion: Our findings suggest that, for the same level of pain, prescription NSAIDs users may experience higher risk of a KR compared to non-users.
 Confounders included demographics, body mass index, Kellgren and Lawrence grade, regular use of prescription opioids, WOMAC stiffness and function scores, objective functional performance measures of chair stand time, 20- and 400-meter walk tests, malalignment, Charlson comorbidity index, Center for Epidemiologic Studies Depression (CES-D) scale, Physical Activity Scale for the Elderly (PASE) score, a knee injury, hip pain or stiffness, and a family history of a knee or a hip replacement.
Confounders included demographics, body mass index, Kellgren and Lawrence grade, regular use of prescription opioids, WOMAC stiffness and function scores, objective functional performance measures of chair stand time, 20- and 400-meter walk tests, malalignment, Charlson comorbidity index, Center for Epidemiologic Studies Depression (CES-D) scale, Physical Activity Scale for the Elderly (PASE) score, a knee injury, hip pain or stiffness, and a family history of a knee or a hip replacement.
To cite this abstract in AMA style:
Jafarzadeh S, Neogi T, Felson D. Long-Term Effect of Prescription Non-Steroidal Anti-Inflammatory Drug Regular Use on the Risk of a Knee Replacement [abstract]. Arthritis Rheumatol. 2021; 73 (suppl 9). https://acrabstracts.org/abstract/long-term-effect-of-prescription-non-steroidal-anti-inflammatory-drug-regular-use-on-the-risk-of-a-knee-replacement/. Accessed .« Back to ACR Convergence 2021
ACR Meeting Abstracts - https://acrabstracts.org/abstract/long-term-effect-of-prescription-non-steroidal-anti-inflammatory-drug-regular-use-on-the-risk-of-a-knee-replacement/
