Session Information
Date: Tuesday, November 14, 2023
Title: (2095–2140) RA – Diagnosis, Manifestations, and Outcomes Poster III
Session Type: Poster Session C
Session Time: 9:00AM-11:00AM
Background/Purpose: Previous studies have highlighted the influence of pain, functional impairment, and affected joint distribution on the discordance in the global assessment of disease activity between patients with rheumatoid arthritis (RA) and their physicians. This study aimed to analyze the effect of affected joint distribution on pain in patients with RA, based on a nationwide RA database in Japan (NinJa).
Methods: The affected joints were divided into four regions: upper-large (shoulder, sternoclavicular, elbow, and wrist), upper-small (proximal interphalangeal and metacarpophalangeal), lower-large (hip, knee, ankle, and tarsometatarsal), and lower-small (metatarsophalangeal) joints. The modified joint index (JI) was calculated using the following formula: number of tender joint counts (instead of the sum of tender and swollen joint counts in the original JI [Rheumatol Int 32:2569, 2012]) divided by the number of evaluable joints within each region. Multiple regression analysis was performed using the pain visual analog scale (VAS) as an objective variable and modified Health Assessment Questionnaire (mHAQ), CRP, and affected joint variables, including JIs and tender joint counts, as explanatory variables.
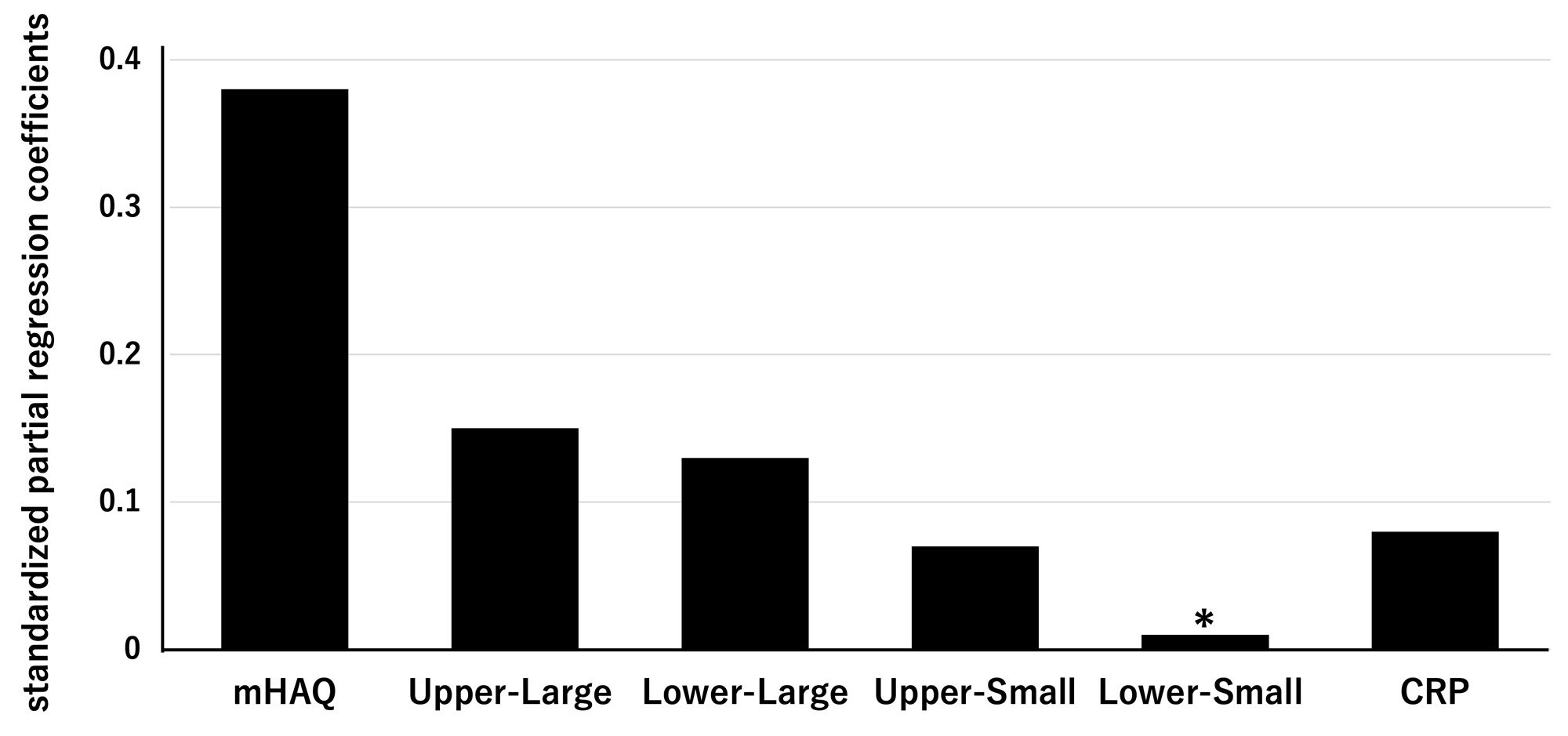
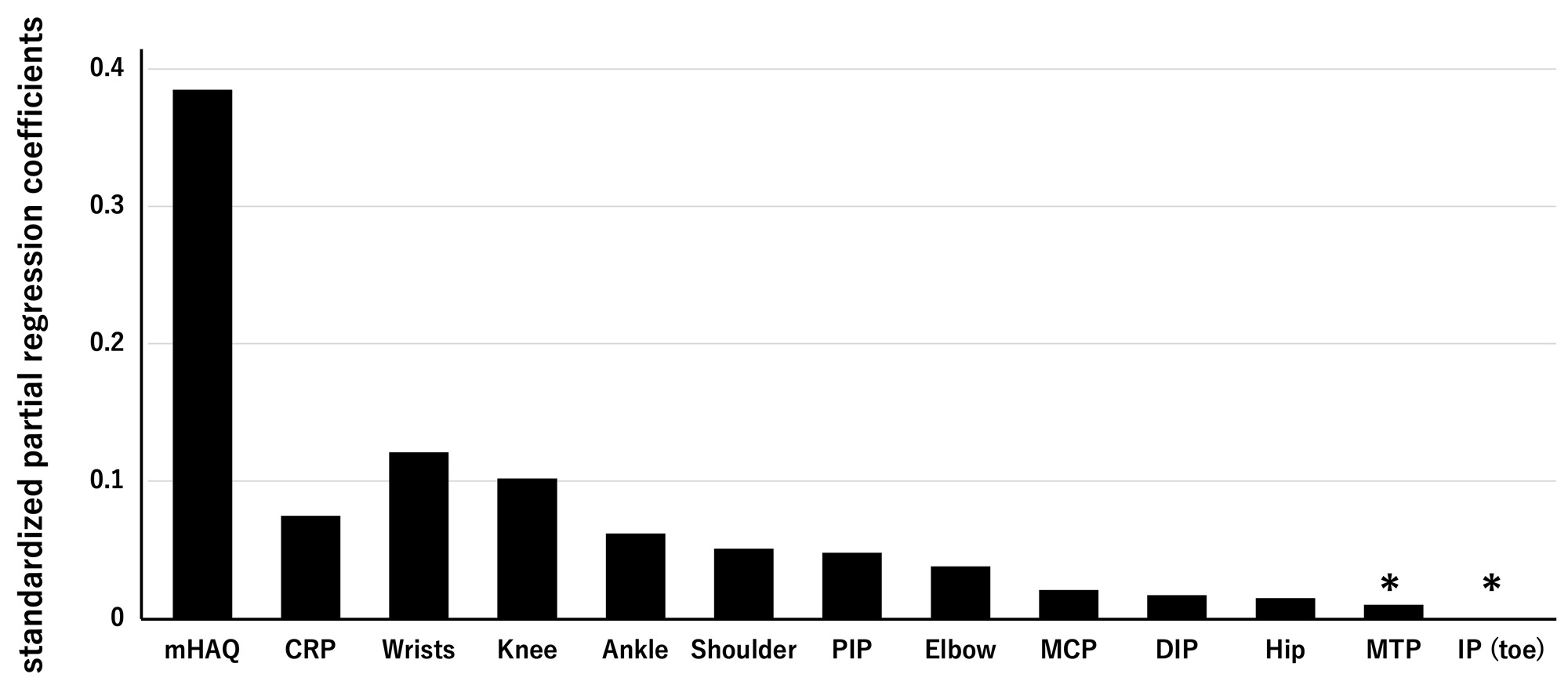
Results: Multiple regression analysis involving 13,653 RA patients revealed that mHAQ, upper-large joints, lower-large joints, CRP, and upper-small joints significantly contributed to pain VAS in the order of standardized partial regression coefficients (SPRCs), although the contribution of lower-small joints was insignificant (Figure 1). Further analysis using tender joint counts showed the impact of each affected joint on pain VAS in the following order of SPRCs: wrists, knees, ankles, shoulders, proximal interphalangeal (PIP) joints, elbows, metacarpophalangeal (MCP) joints, distal interphalangeal (DIP) joints, and hips (Figure 2). Notably, the effects of metatarsophalangeal (MTP) and toe interphalangeal (IP) joints, which were excluded from the disease activity score-28 (DAS28), were not statistically significant.
Conclusion: The effect of lower-small joint involvement on pain in RA is smaller than that of upper-small joint involvement. Thus, patients with RA are relatively less aware of MTP and toe IP joint pain as compared to PIP and MCP joints, and may not complain to their physicians, which could lead to forefoot joint deformities. Therefore, it is necessary to consider lower-small joint involvement, which is not included in DAS28 evaluation, and pay attention to its potential impact on management in RA patients.
To cite this abstract in AMA style:
Sawada T, Nishiyama S, Igari S, Matsui T, Tohma S. Lesser Impact of Lower-Small Joint Involvement on Pain Than Upper-Small Joint in Rheumatoid Arthritis: Analysis Based on a Large Rheumatoid Arthritis Database in Japan [abstract]. Arthritis Rheumatol. 2023; 75 (suppl 9). https://acrabstracts.org/abstract/lesser-impact-of-lower-small-joint-involvement-on-pain-than-upper-small-joint-in-rheumatoid-arthritis-analysis-based-on-a-large-rheumatoid-arthritis-database-in-japan/. Accessed .« Back to ACR Convergence 2023
ACR Meeting Abstracts - https://acrabstracts.org/abstract/lesser-impact-of-lower-small-joint-involvement-on-pain-than-upper-small-joint-in-rheumatoid-arthritis-analysis-based-on-a-large-rheumatoid-arthritis-database-in-japan/