Session Information
Date: Sunday, October 21, 2018
Title: Systemic Lupus Erythematosus – Clinical Poster I: Clinical Manifestations and Comorbidity
Session Type: ACR Poster Session A
Session Time: 9:00AM-11:00AM
Background/Purpose: Lupus Nephritis (LN) usually presents within 5 years of SLE diagnosis, however the minority of patients with late-occurring nephritis are poorly characterized. Factors associated with high risk for early nephritis include male gender, Hispanic and African American race, and childhood-onset SLE (Jacobsen et. al. 1998, Seligman et. al. 2002). Since proliferative nephritis is a more aggressive class of nephritis than membranous and mesangial nephritis, we hypothesized that female gender, Caucasian race, adult-onset SLE, and membranous pathology would be associated with a later or more insidious onset of nephritis.
Methods: A single large urban medical center was the source for retrospective record review of patients who underwent kidney biopsy between 1999 and 2015. Patients with biopsy-proven LN were evaluated to determine whether gender, race, age at SLE diagnosis, age at first biopsy, or histopathologic classification were associated with the time (years) between SLE diagnosis and first renal biopsy.
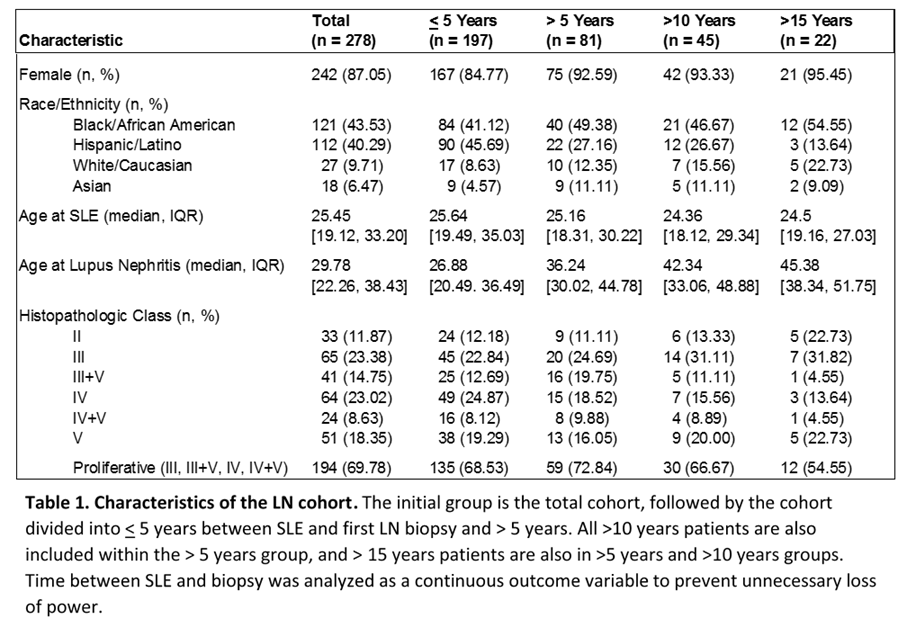
Results: 630 patients were screened. After elimination of duplicates, those without initial biopsy, biopsy findings other than lupus nephritis, and unknown date of SLE diagnosis, 293 subjects had adequate data available for analysis. Those with late onset SLE, diagnosis after age 50 (n=15), were excluded from further analysis due to known differences in this subgroup. The remaining 278 patients had characteristics shown in Table 1. Twenty-nine percent of patients in this cohort developed nephritis more than 5 years after initial SLE diagnosis, including 50% of Asian, 37% of Caucasian, 33% of African American, and 20% of Hispanic LN patients. Multivariable linear regression identified greater age at first biopsy and race as the strongest predictors of time between SLE diagnosis and first renal biopsy. Hispanic patients were more likely to present with LN earlier in their course and Asian patients were more likely to present later, with African American and Caucasian groups between them. The model accounts for 27% of the variability in the time elapsed between diagnosis and biopsy. Histopathologic class did not make a significant contribution, and proliferative nephritis was noted in similar numbers of patients who developed LN after 5 years (73%) and those in the early presenting group (69%, p=0.6).
Conclusion: Surprisingly, more than a quarter of known LN patients at this large US center present after 5 years of SLE, higher than expected based on low numbers of late onset nephritis in other cohorts. This appears to be more common in Caucasian and Asian subgroups. Older patients are more likely to develop nephritis later, but aggressive histopathology is not less likely in later presentations. The data underscore the importance of remaining vigilant about nephritis risk in patients of diverse demographics five years and more after diagnosis with SLE.
To cite this abstract in AMA style:
Arriens C, Chen S, Karp D, Saxena R, Merrill JT, James JA. Is Lupus Nephritis Onset Delayed in Older Caucasian Females with Less Aggressive Pathology? [abstract]. Arthritis Rheumatol. 2018; 70 (suppl 9). https://acrabstracts.org/abstract/is-lupus-nephritis-onset-delayed-in-older-caucasian-females-with-less-aggressive-pathology/. Accessed .« Back to 2018 ACR/ARHP Annual Meeting
ACR Meeting Abstracts - https://acrabstracts.org/abstract/is-lupus-nephritis-onset-delayed-in-older-caucasian-females-with-less-aggressive-pathology/