Session Information
Session Type: Poster Session B
Session Time: 10:30AM-12:30PM
Background/Purpose: Pyrexia of Unknown Origin (PUO) is defined as a fever above 38.3°C recorded on several occasions, that evades diagnosis for at least 3 weeks. PUO remains a clinical challenge for many physicians and frequently needs multi-speciality input, often from rheumatology, infectious diseases, and haematology. There have been no recent studies on large volume PUO cohorts. Therefore, our study aims to review the PUO investigative pathway with a particular focus on the role and input of the rheumatologist.
Methods: We performed a retrospective analysis of all patients who underwent investigations for PUO between January 2020 and October 2022 at a single tertiary central London hospital. Data were extracted from electronic healthcare records. We reviewed patient demographics, numbers of haematological, biochemical, autoimmune, inflammatory and infection screens, and radiological scans, including whole body imaging, and biopsies. The frequency of involvement of specialist clinicians and final diagnoses were also reviewed.
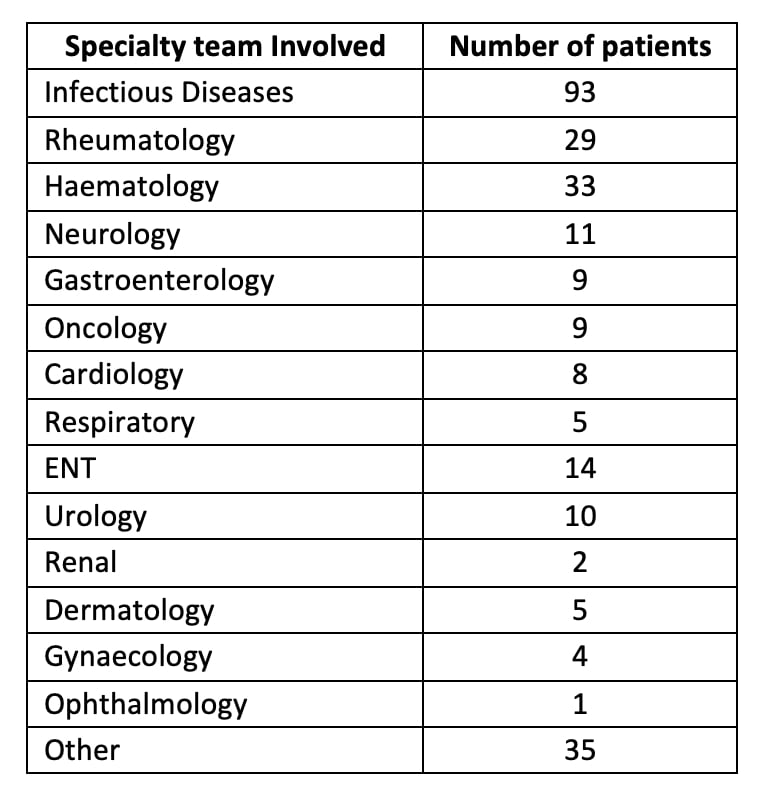
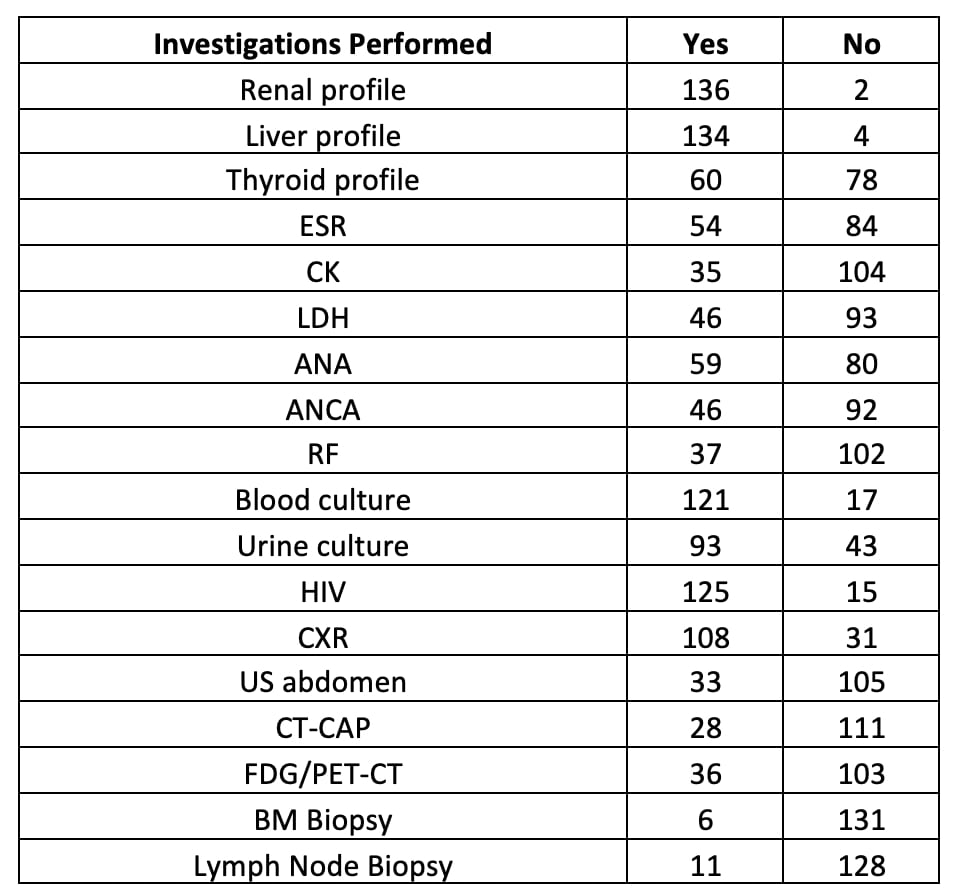
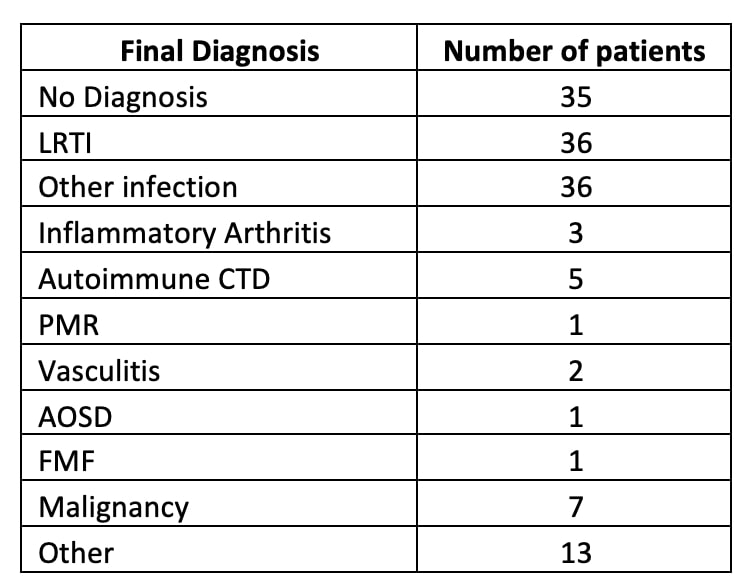
Results: A total of 140 patients met the inclusion criteria. The most common age group to present with a PUO was 31–40 year-olds (38, 27.1%), of equal gender distribution and of Caucasian ethnicity (64, 45.7%). 23 patients (16.4%) were of Asian ethnicity, 20 (14.3%) were Afro-Caribbean, and the remainder (33, 23.6%) of other or unknown ethnicity. The majority of patients (95, 67.9%) presented via the emergency department; three (2.1%) had their first evaluation in the rheumatology clinic. Overall, the rheumatology team was involved in 29 cases (20.7%). 32 patients (22.9%) saw 3 or more specialist clinicians, the infectious diseases team being most frequently involved (93, 66.4%), followed by haematology (33, 23.6%) and rheumatology (Table 1). Autoimmune screens were sent, including anti-nuclear antibodies (ANA) for 59 patients (42.1%), anti-neutrophil cytoplasmic antibodies (ANCA) for 46 (32.9%), and rheumatoid factor (RF) for 37 (26.4%). 36 patients (25.7%) had FDG-PET/CT. 43 patients (30.7%) underwent biopsies, most frequently lymph node (11, 7.9%) and bone marrow (6, 4.3%) (Table 2). 13 patients (9.3%) received a rheumatologic diagnosis. The most frequent diagnoses were infections (72, 50.7%), including viral, bacterial respiratory tract, and urinary tract infections. No final diagnosis was reached for 35 patients (25%) (Table 3).
Conclusion: This retrospective study supports that careful assessment by the rheumatology team remains an important part of the work-up of a patient with PUO. It is striking that even with unlimited access to diagnostic testing, the cause of PUO remains elusive in a significant minority of patients, as reported in the literature historically (1).
References
1. Fernandez C, Beeching NJ. Pyrexia of unknown origin. Clin Med (Lond). 2018 Mar;18(2):170-174. doi: 10.7861/clinmedicine.18-2-170. PMID: 29626024; PMCID: PMC6303444.
ENT = Ears, Nose and Throat
ESR = erythrocyte sedimentation rate; CK = creatine kinase; LDH = lactate dehydrogenase; ANA = anti-nuclear antibodies; ANCA = antineutrophil cytoplasmic antibody; RF = rheumatoid factor; HIV = human immunodeficiency virus; CXR = chest radiograph, US = ultrasound; CT-CAP= computed tomography chest abdomen and pelvis; FDG/PET-CT = fluorodeoxyglucose positron emission tomography/computed tomography; BM = bone marrow
LRTI = lower respiratory tract infections; CTD = connective tissue disease; PMR = Polymyalgia Rheumatica; AOSD= Adult-Onset Still’s Disease; FMF = Familial Mediterranean Fever
To cite this abstract in AMA style:
Moezinia C, Nouza J, Hornstein-Lasry B, Kawar L, Khan A, Manson J. Investigating Pyrexia of Unknown Origin: A Rheumatologist’s Perspective [abstract]. Arthritis Rheumatol. 2024; 76 (suppl 9). https://acrabstracts.org/abstract/investigating-pyrexia-of-unknown-origin-a-rheumatologists-perspective/. Accessed .« Back to ACR Convergence 2024
ACR Meeting Abstracts - https://acrabstracts.org/abstract/investigating-pyrexia-of-unknown-origin-a-rheumatologists-perspective/