Session Information
Date: Tuesday, November 14, 2023
Title: (2257–2325) SLE – Diagnosis, Manifestations, & Outcomes Poster III
Session Type: Poster Session C
Session Time: 9:00AM-11:00AM
Background/Purpose: Type I Interferons (IFN-I) play a role in SLE and Lupus Nephritis (LN) pathogenesis. We have recently shown that IFN-I gene expression predicts the risk of SLE flares and a more severe disease course in SLE patients. Furthermore, recently it has been suggested that patients with higher IFN-I gene expression in their renal tubular cells are less likely to respond to conventional therapy.
The aim of this study was to determine if the amount of IFN-α in serum at the time of an LN flare predicts response to therapy, subsequent LN flares, and decline in kidney function.
Methods: Patients with active LN were included in this study. All patients had 1) active LN, defined as a 24H urine protein >500mg/day with a subsequent modification in therapy by the treating physician, 2) stored serum sample ±3 months from the renal flare and 3) baseline estimated glomerular filtration rate (eGFR) ≥60ml/min (3 months prior to the flare).
The following outcomes were ascertained: 1) Complete Response (CR), defined as proteinuria < 500 mg/day and a serum creatinine within 15% of the baseline at 1 and 2 years after the flare, 2) number of LN flares during follow-up (defined by an increase in proteinuria of at least 1000 mg/d if the baseline was < 500 mg/d or doubling of proteinuria in baseline was ≥500 mg/d and a change in therapy by the treating physician, and 3) decline in eGFR to ≤59ml/min, ≤44ml/min,≤29ml/min and < 15ml/min during follow-up.
Serum IFN-α was measured by Simoa®
Results: A total of 95 patients with active LN were included in the study. The median (IQR) age of the patients was 29 (23-41) years, 79 (83.7%) were women, and the disease duration was 6.0 (0.2-10.0) years. Forty (42.1%) were Caucasian, 21 (22.1%) were Afro-Caribbean, and 22 (23.1.%) were Asian. The baseline eGFR was 112 (98.7-127) ml/min, and the median (IQR) follow-up was 132 (96-156) months.76.8% had a kidney biopsy at the time of the LN flare, of whom 54.7% had a proliferative or mixed class, 17.8% class V, and 4.2% class I or II. The median (IQR) of prednisone was 40mg (30-38mg), 89 (93%) received antimalarial and all patients received immunosuppressive therapy.
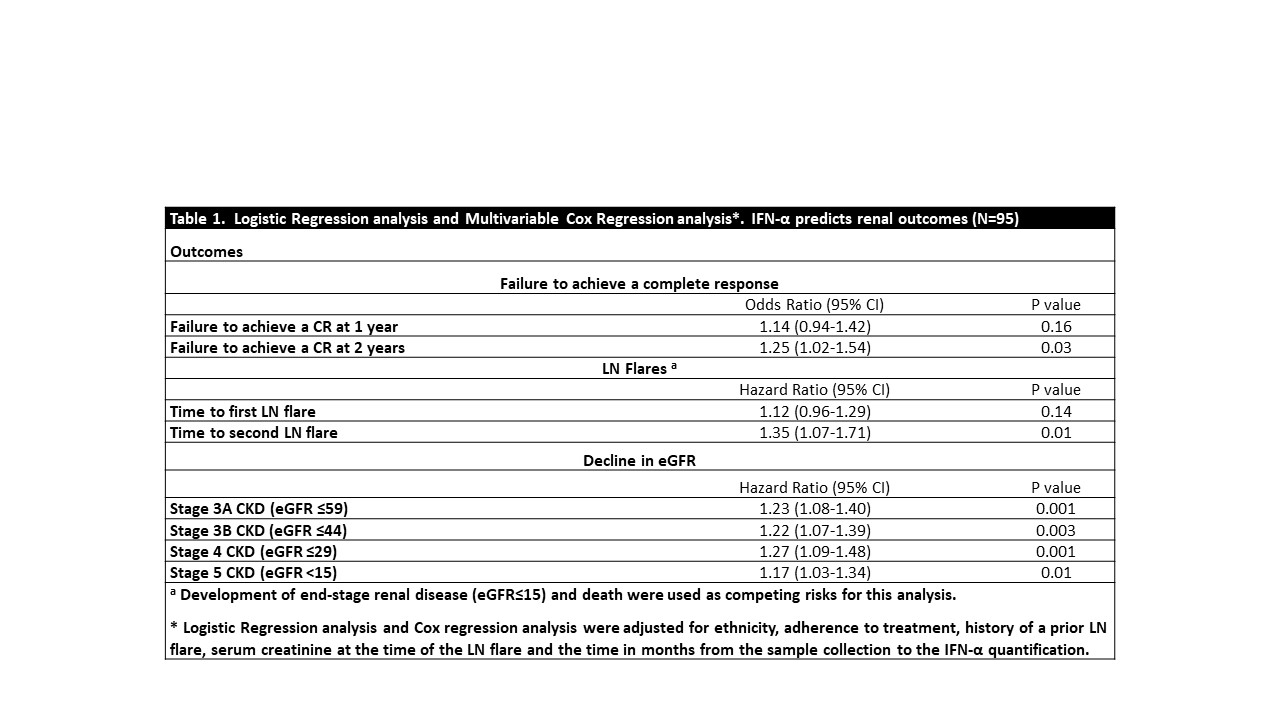
The serum baseline levels of IFN-α predicted CR at 2 years from the LN flare. Furthermore, patients with higher baseline levels of IFN-α had a greater risk of having 2 or more subsequent renal flares. Every increase in 1 unit of IFN-α increased the risk of having 2 or more flares by 35%, and the risk of having a decline in kidney function during follow-up (Table 1).
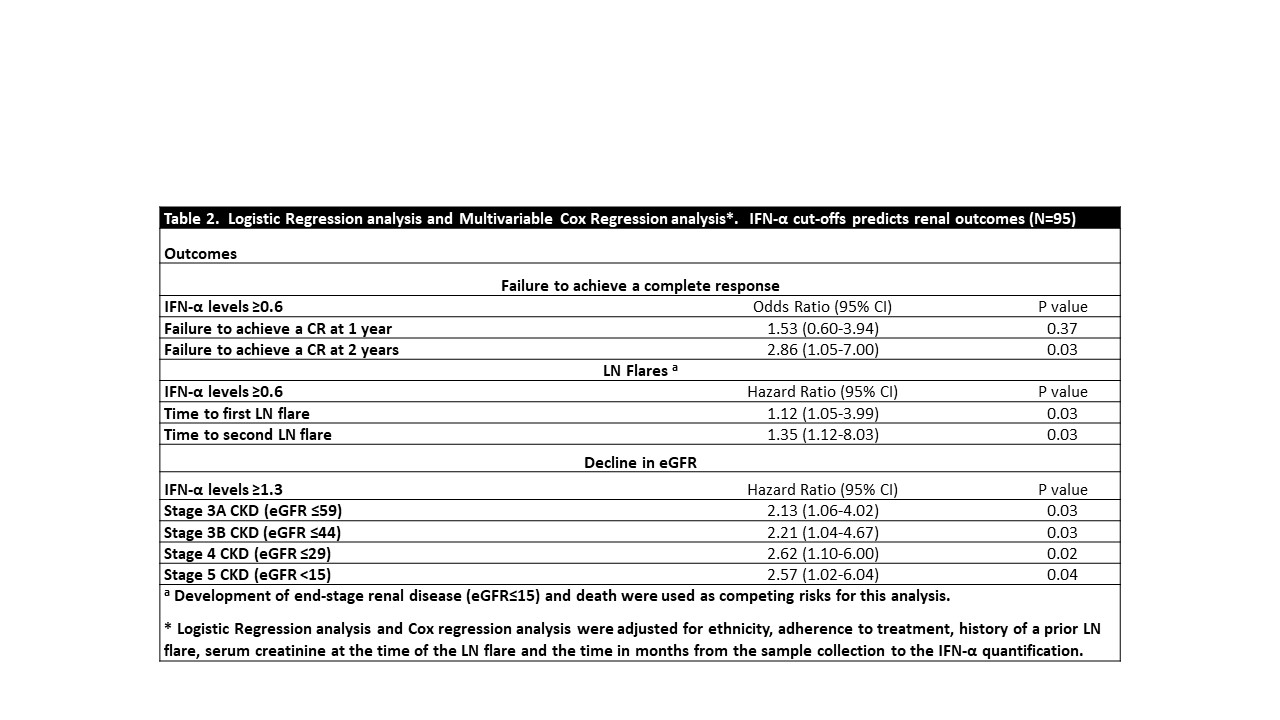
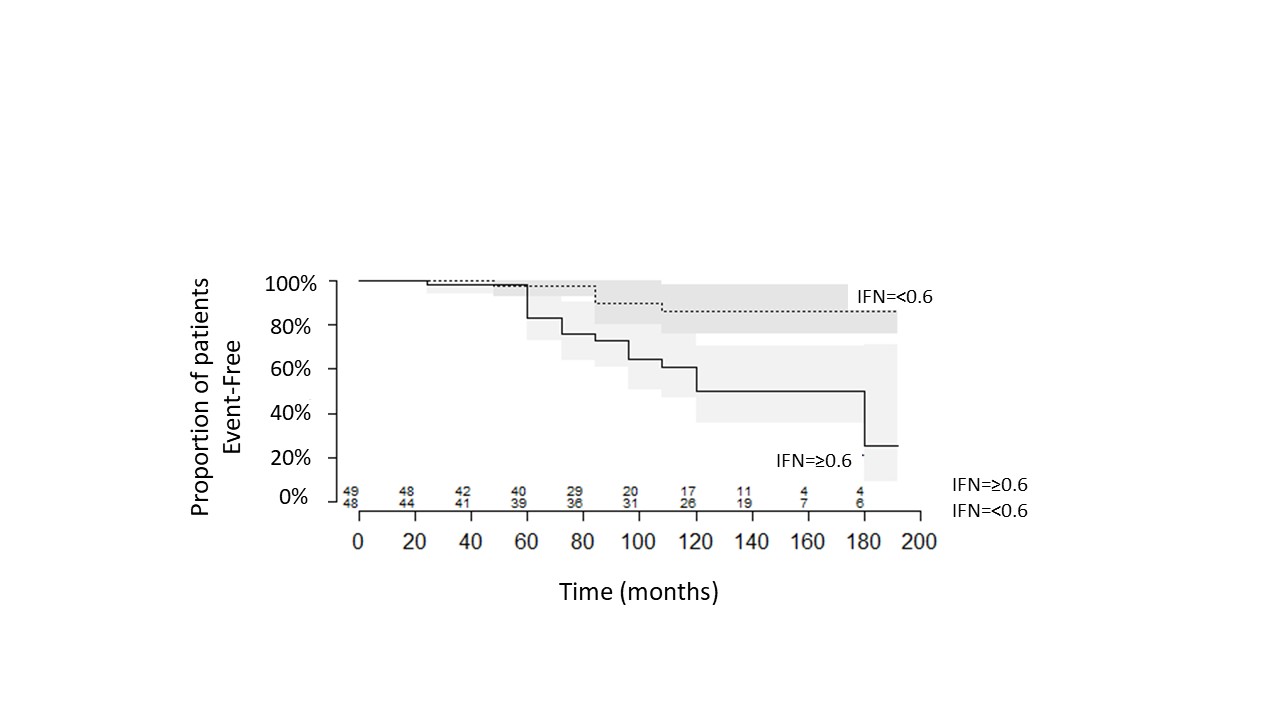
Using ROC analysis, two IFN-α cut-offs were identified, 0.6 and 1.3 for predicting ≥2 LN flares and progression to eGFR ≤15, respectively. Even though the areas under the curve suggested that IFN-α is only a weak predictor (AUC=0.62 (0.51-0.74) and 0.60 (0.47-0.73) for ≥2 LN flares and progression to eGFR ≤15, respectively), these cutoffs continued to predict renal outcomes on Cox regression analysis, as seen in Figure 2 and Table 2.
Conclusion: IFN-α serum levels predicted failure to respond to treatment at year 2 after the renal flare, the development of ≥2 LN flares, and decline in kidney function during follow-up.
To cite this abstract in AMA style:
Whittall Garcia L, Gladman D, Urowitz M, Touma Z, Wither J. Interferon-α as a Biomarker to Predict Flares in Lupus Nephritis [abstract]. Arthritis Rheumatol. 2023; 75 (suppl 9). https://acrabstracts.org/abstract/interferon-%ce%b1-as-a-biomarker-to-predict-flares-in-lupus-nephritis/. Accessed .« Back to ACR Convergence 2023
ACR Meeting Abstracts - https://acrabstracts.org/abstract/interferon-%ce%b1-as-a-biomarker-to-predict-flares-in-lupus-nephritis/