Session Information
Session Type: Poster Session A
Session Time: 10:30AM-12:30PM
Background/Purpose: Minoritized individuals with systemic lupus erythematosus (SLE) experience social determinants of health (SDOH) challenges that affect access to care and increase the risk for poorer outcomes in SLE1. Medical teams lack expertise, time, and resources to effectively address SDOH. After a pilot phase identified high volume and complexity of SDOH needs in the SLE patient population, we implemented an integrated multidisciplinary rheumatology/nephrology Lupus Social Work Program (LSWP) to manage SDOH for participants with SLE and lupus nephritis (LN).
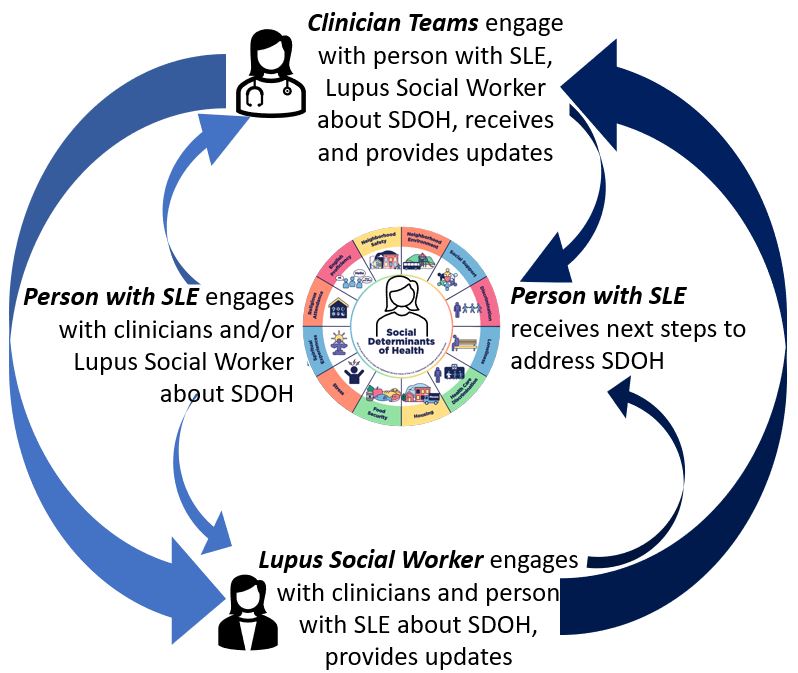
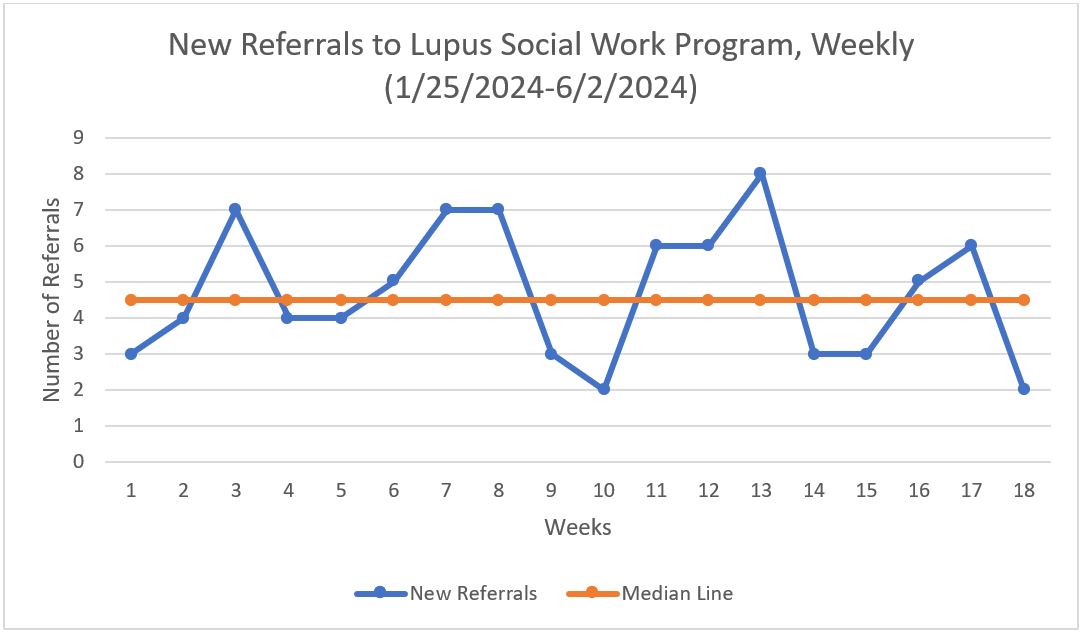
Methods: In the pilot phase (abstract 1856027), volunteer community navigators identified frequent and complex financial and social needs for 28 participants with SLE. In response to this identified need, we developed an integrated multidisciplinary LSWP to manage SDOH in outpatient and inpatient settings in the rheumatology and nephrology divisions at an academic center. Between January and June of 2024, clinicians referred participants with SLE to a licensed social worker prioritized by high social need, disease activity, and disease severity, including LN. Referrals from clinicians through the electronic medical record (EMR) system included a trackable data element that then populated a LWSP dashboard. The lupus social worker, whose caseload was exclusive to SLE, connected with patients via text, call, EMR messaging, and in person meetings. The social worker documented assessments in the EMR and managed SDOH by providing resources. Cases were discussed in weekly meetings with the social worker, nephrologists, rheumatologists, and administrative personnel (Figure 1). Using the Children’s Hospital of Philadelphia Leading Improvement Framework, the early primary aim was to develop a workflow to increase referrals to the LSWP to 10 referrals/month for 4.5 months (1/2024-6/2024), independent of participant ancestry, insurance status, language, or beliefs. For each patient, the type of SDOH and subsequent interventions were recorded.
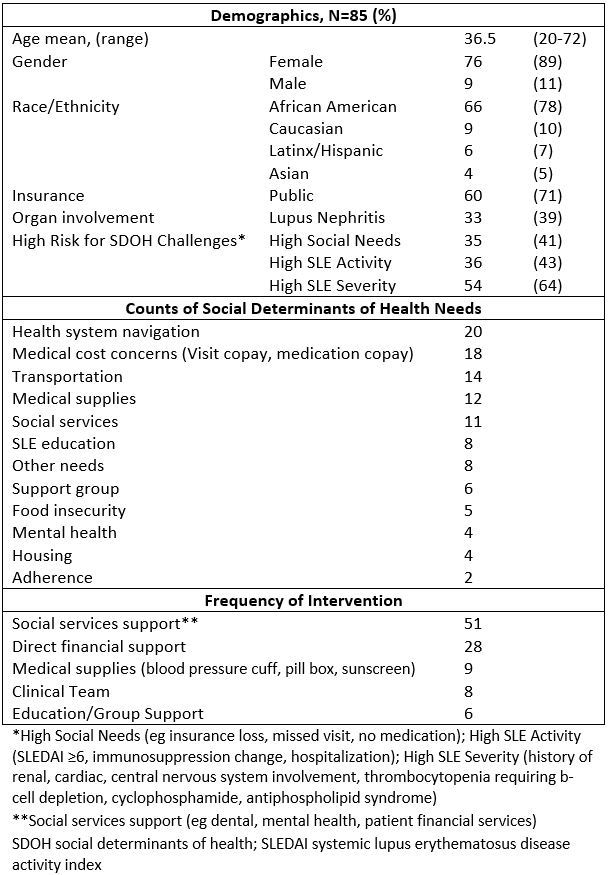
Results: There were 85 referrals in 18 weeks, or 19/month, exceeding the aim of 10/month (Figure 2). There were 177 LSWP encounters with documented SDOH averaging 2 encounters/referral. Most referrals were for young women (89%, 76/85) who self-identified as African American (78%, 66/85) (Table). Thirty nine percent (33/85) of participants had LN, over half (55%, 18/33) of whom had high social needs. Most frequent SDOH needs were health system navigation (20) and cost concerns (18). The top 2 interventions were social services support (51) and direct financial support (28). Twenty two percent of patients (19/85) were not reached.
Conclusion: The integrated multidisciplinary Lupus Social Work Program generated 85 referrals in the first 4.5 months, exceeding the initial aim. No answer to the initial outreach was frequent, suggesting repeated multimodal efforts are needed for a subset. For people with SLE at high risk for poor outcomes, an integrated lupus social work expert can manage a high volume of complex SDOH that may be under-addressed by clinical teams.
1Aguirre J Rheumatol 2023 PMID 37321640.
We acknowledge Michele Taylor for her contributions to this abstract.
To cite this abstract in AMA style:
DeQuattro K, DeVaughn S, Kanoff A, Geara A. Integrated Multidisciplinary Lupus Social Work Program to Manage Social Determinants of Health in SLE and Lupus Nephritis – Preliminary Results [abstract]. Arthritis Rheumatol. 2024; 76 (suppl 9). https://acrabstracts.org/abstract/integrated-multidisciplinary-lupus-social-work-program-to-manage-social-determinants-of-health-in-sle-and-lupus-nephritis-preliminary-results/. Accessed .« Back to ACR Convergence 2024
ACR Meeting Abstracts - https://acrabstracts.org/abstract/integrated-multidisciplinary-lupus-social-work-program-to-manage-social-determinants-of-health-in-sle-and-lupus-nephritis-preliminary-results/