Session Information
Session Type: Poster Session A
Session Time: 10:30AM-12:30PM
Background/Purpose: Antineutrophilic cytoplasmic antibody (ANCA)-associated vasculitides (AAV) are a heterogeneous group of rare autoimmune conditions characterized by inflammation of blood vessels, leading to various clinical manifestations. This group includes three main diseases: granulomatosis with polyangiitis (GPA), eosinophilic granulomatosis with polyangiitis (EGPA), and microscopic polyangiitis (MPA). In this study, we conducted a retrospective database analysis to compare the outcomes among these three major types of AAV.
Methods: We utilized the NIS from 2016-2020 to identify patients affected by granulomatosis with polyangiitis (GPA), eosinophilic granulomatosis with polyangiitis (EGPA), and microscopic polyangiitis (MPA) using their pertinent ICD-10 codes. Our study included all individuals with a primary or secondary diagnosis of EGPA, MPA, or GPA above the age of 18. We outlined their sociodemographic features and analyzed inpatient outcomes, including but not limited to mortality, gastrointestinal, cardiac, and renal involvement, using logistic regression.
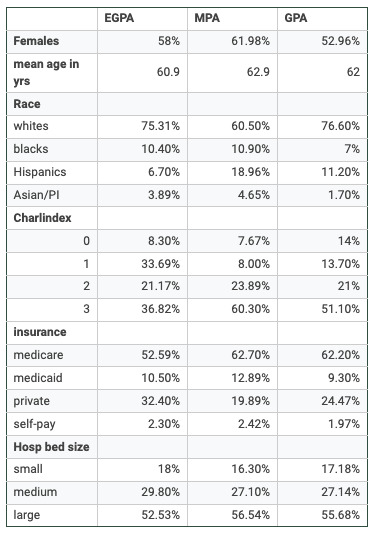
Results: There were a total of 76,389 patients with AAV, including 58,474 with GPA, 11,805 with MPA, and 8,784 with EGPA. Baseline characteristics are outlined below in a tabulated form.
Patients with MPA had a longer hospital stay (mean – 9.1 days) compared to those with EGPA (6.3 days) and GPA (7.01 days). The cost burden was also higher for MPA patients ($123,241.2) compared to those with EGPA ($78,023.3) and GPA ($90,118.1).
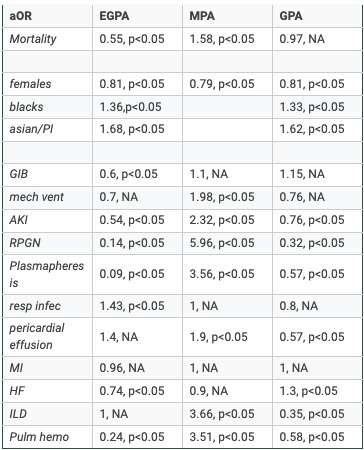
MPA patients had higher odds of inpatient mortality compared to those with GPA or EGPA (OR 1.58, p< 0.05). And stratification revealed that males had higher odds across all cohorts (p< 0.05), and Blacks & Asians had higher odds in the EGPA (1.36;1.68) and GPA cohort (1.33;1.62), respectively, p< 0.05.
EGPA patients had lower odds of GI bleeding (OR 0.6, p< 0.05). MPA patients had nearly double the odds of requiring mechanical ventilation (OR 1.98, p< 0.05). The OR for AKI in MPA patients was 2.32 compared to GPA or EGPA (p< 0.05). Compared to MPA and GPA, EGPA patients had higher odds of acquiring respiratory infections (OR 1.43, p< 0.05). MPA patients had higher odds of pericardial effusion (OR 1.9, p< 0.05), RPGN (OR 5.96, p< 0.05) & requiring plasmapheresis (OR 3.56, p< 0.05).
While the odds for MI were not statistically significant, GPA patients had higher odds of heart failure compared to those with MPA or EGPA (OR 1.3, p< 0.05). MPA patients also had higher odds of developing ILD (OR 3.66, p< 0.05) and pulmonary hemorrhage (OR 3.51, p< 0.05).
Conclusion: Our comprehensive study on AAV patients, including GPA, MPA, and EGPA subtypes, revealed significant clinical and demographic disparities. MPA patients, who experienced longer hospital stays, higher costs, and increased mortality risk, highlight the critical need for targeted interventions. Our study also revealed specific comorbidity patterns, such as higher odds of AKI and pulmonary hemorrhage in MPA, and greater heart failure risk in GPA patients. These findings underscore the importance of timely identification and intervention for patients with AAV.
To cite this abstract in AMA style:
Pannala S, Saliba f, Rajamanuri M, Katikineni V. Inpatient Outcomes in ANCA-Associated Vasculitis: An In-Depth Cross-Sectional Analysis Using NIS Data (2016-2020) [abstract]. Arthritis Rheumatol. 2024; 76 (suppl 9). https://acrabstracts.org/abstract/inpatient-outcomes-in-anca-associated-vasculitis-an-in-depth-cross-sectional-analysis-using-nis-data-2016-2020/. Accessed .« Back to ACR Convergence 2024
ACR Meeting Abstracts - https://acrabstracts.org/abstract/inpatient-outcomes-in-anca-associated-vasculitis-an-in-depth-cross-sectional-analysis-using-nis-data-2016-2020/