Session Information
Session Type: Poster Session B
Session Time: 10:30AM-12:30PM
Background/Purpose: Hospitalizations for gout flare have been increasing, doubling between 1993 to 2011 from 4.4 to 8.8 admissions per 100000 adults. Despite this increase, urate-lowering therapy (ULT) prescription has remained stagnant for decades. The 2020 ACR Guideline for the Management of Gout (GMG) provides 3 indications for initiating ULT based on strength of recommendation and quality of evidence: ≥2 flares/y, tophaceous gout, or radiographic damage (indication 1, strongly recommended with high-moderate certainty); >1 flare but < 2 flares/y (indication 2, conditionally recommended with moderate certainty); first flare with chronic kidney disease (CKD) ≥3, serum urate >9 mg/dL, or urolithiasis (indication 3, conditionally recommended with very low certainty). We performed a retrospective analysis assessing number of gout flare hospitalizations, number of ULT-naive patients hospitalized with gout flare meeting each of the 3 indications, and our institution’s practice of initiating ULT in these patients. Our objective is to use this data to determine current practice at our institution and create a specific plan-do-study-act (PDSA) cycle protocol to optimize prescription of ULT among these patients.
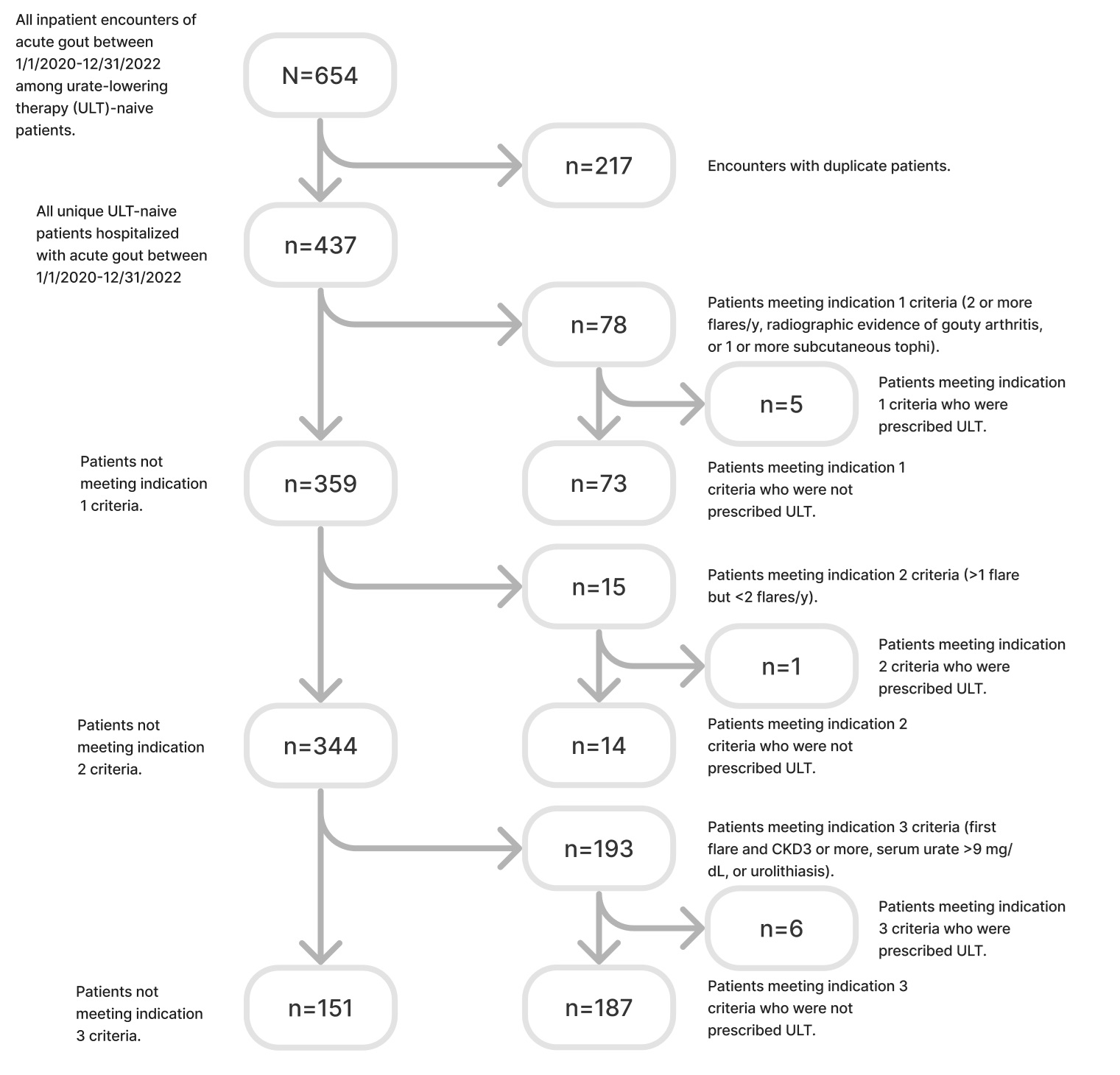
Methods: We collected data through Michigan Data Analytics for patients hospitalized at Trinity Health Grand Rapids (THGR) between 1/1/20-12/31/22 with diagnosis of acute gout (ICD-10 code M10) who were previously not on ULT (i.e., allopurinol, febuxostat, and probenecid). This included data on demographics, glomerular filtration rate (GFR), and whether ULT was prescribed at discharge. Duplicate patients were omitted. Patients were sequentially stratified into groups based on whether they met one of the 3 indications for ULT per the 2020 ACR GMG (Figure 1). One-way ANOVA compared age and GFR differences among the 3 groups. The Fisher’s exact test compared ULT initiation and Pearson Χ2 tests compared sex and race differences among the groups. A survey assessing knowledge of gout management was sent to 20 THGR internal medicine (IM) residents.
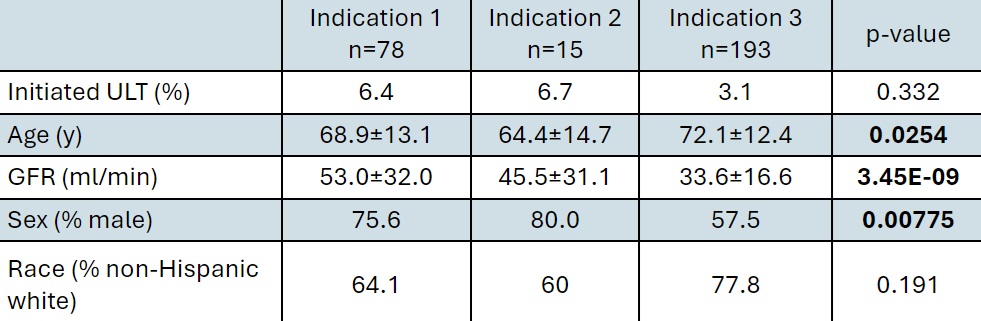
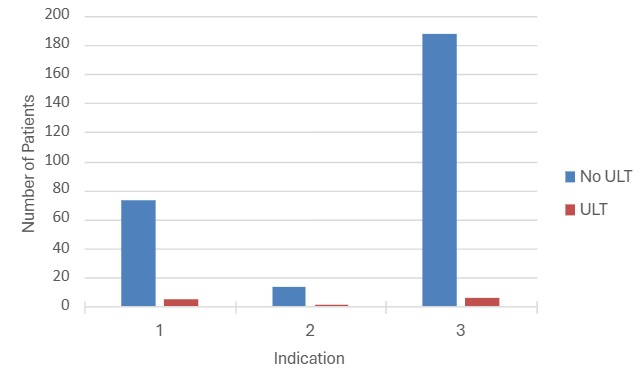
Results: Of 437 unique patients hospitalized with acute gout during the studied period at our institution, 78 met indication 1, 15 met indication 2, and 193 met indication 3 for ULT (Figure 2). Only 12 patients were prescribed ULT by discharge. There was a significant difference in age (F(2,283)=3.72, p=.0254), GFR (F(2,283)=20.89, p=3.45×10-9), and sex (X2(2,N=286)=9.72, p=.00775) among the 3 indication groups (Table 1). ULT initiation and race were similar among the groups. Survey results revealed 20% of residents identifying types of ULT and 0% identifying the 3 indications for ULT per the 2020 ACR GMG.
Conclusion: Our analysis shows that inpatient ULT initiation in ULT-naive patients hospitalized with gout flare who met one of the 3 indications per the 2020 ACR GMG is poor. Knowledge assessment among IM residents is similarly poor. A quality improvement project using the PDSA cycle is being initiated at our institution to improve inpatient ULT initiation, first focusing on indication 1. Next steps include using pharmacists to remind providers to prescribe ULT in patients who have been hospitalized with ≥2 flares/y and increasing provider education and awareness.
To cite this abstract in AMA style:
Nasir A, Khan N. Initiation of Urate-Lowering Therapy in Patients Hospitalized with Gout Flare at a Single Center: Opportunity for Quality Improvement [abstract]. Arthritis Rheumatol. 2024; 76 (suppl 9). https://acrabstracts.org/abstract/initiation-of-urate-lowering-therapy-in-patients-hospitalized-with-gout-flare-at-a-single-center-opportunity-for-quality-improvement/. Accessed .« Back to ACR Convergence 2024
ACR Meeting Abstracts - https://acrabstracts.org/abstract/initiation-of-urate-lowering-therapy-in-patients-hospitalized-with-gout-flare-at-a-single-center-opportunity-for-quality-improvement/