Session Information
Session Type: Poster Session B
Session Time: 9:00AM-11:00AM
Background/Purpose: Infrared thermography (IRT) is an emerging technology that has the potential to rapidly assist in identifying joint inflammation in patients with joint symptoms. However, its use in clinical practice is currently limited due to the lack of a true gold standard (e.g., musculoskeletal ultrasound [MSUS]) confirming the presence of joint inflammation. We aimed to determine whether there are differences in IRT measurements between joints categorized as inflamed or not based on Power Doppler (PD) ultrasound imaging.
Methods: We conducted a cross sectional study among patients at a tertiary academic medical center. Eligible patients were age ≥ 18 years, had a rheumatologist-diagnosis of rheumatoid arthritis or a non-inflammatory joint condition (e.g. osteoarthritis) or healthy controls, and had at least one swollen joint in the hands or wrists or feet (RA patients only). IRT images were obtained using a FLIR E75 3400 camera. A manual segmentation approach was employed to place rectangular regions of interests (ROIs) over each of the 32 target joint sites. FLIR software was used to determine IRT temperature (0C) parameters including ROI maximum (max), minimum (min), mean (mean), center (center) and within joint variability (STD). MSUS was obtained at the same visit by a rheumatologist with RhMSUS certification. MSKUS erosions (presence/absence), joint inflammation (PD) and synovial hypertrophy (SHT) was scored using a 0-3 severity scale (none =0, mild =1, moderate=2, and severe =3) for each wrist, metacarpophalangeal (MCP), proximal interphalangeal (PIP) and metatarsophalangeal (MTP) joint. We used mixed effects logistic regression to determine whether IRT parameters were able to discriminate between inflamed (i.e. PD score ≥ 1) and not inflamed joints (PD=0), accounting for clustering of joints within patients and adjusting for demographic factors including age, sex, and race.
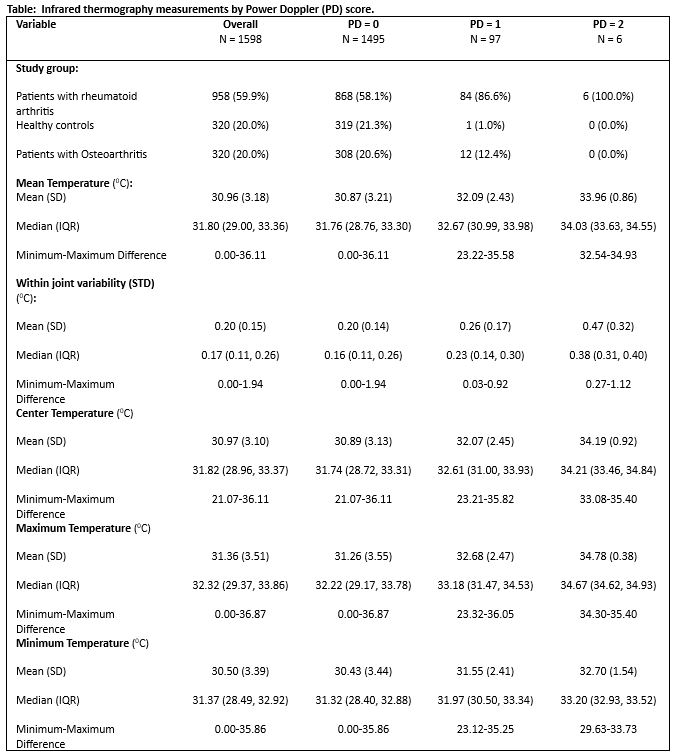
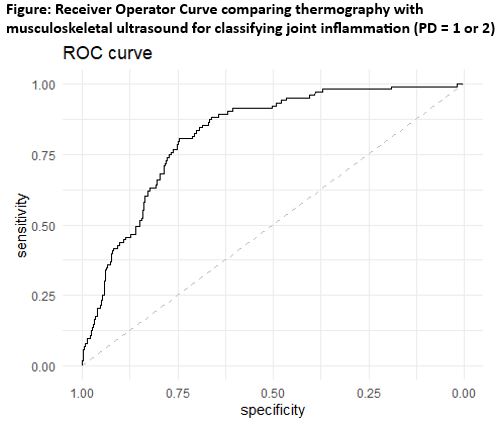
Results: A total of 50 patients with RA (n=30), OA (n=10), healthy controls mean (SD) age 54.8 (14.20) years, mostly women (90.0%), 22 (44%) Black participated in the study. A total of 1598 joints were included in the analysis including 103 joints with a PD ≥ 1. A total of 248 joints had erosions. IRT measurements by PD score are presented in the Table. The c-statistic for the area under the receiver operator curve was 0.82 (Figure). After multivariable adjustment, the minimum, maximum and the within-joint variability (STD) of the thermography camera temperature readings were significantly associated with joint inflammation compared to the gold standard of PD={1,2} by MSUS. Older age, female sex, and black race also were significantly associated with the outcome.
Conclusion: We found that a commercially-available infrared thermography camera had reasonable accuracy to discriminate between inflamed versus non-inflamed joints among people with RA, OA, and healthy controls. These findings can help inform future use of IRT in clinical practice to discriminate between inflammatory and non-inflammatory joint disease in settings where a rheumatologist physical exam may not be feasible.
To cite this abstract in AMA style:
Danila M, Rosas G, Xie F, Curtis J, Aaron K, Ford S, Hughes L. Infrared Thermography Imaging Discriminates Between Inflamed and Non-inflamed Joints [abstract]. Arthritis Rheumatol. 2023; 75 (suppl 9). https://acrabstracts.org/abstract/infrared-thermography-imaging-discriminates-between-inflamed-and-non-inflamed-joints/. Accessed .« Back to ACR Convergence 2023
ACR Meeting Abstracts - https://acrabstracts.org/abstract/infrared-thermography-imaging-discriminates-between-inflamed-and-non-inflamed-joints/