Session Information
Session Type: Poster Session A
Session Time: 10:30AM-12:30PM
Background/Purpose: Orbital inflammatory diseases in the pediatric population present diagnostic and therapeutic challenges due to variable clinical manifestations, limited prospective data, and lack of standardized treatment protocols. This case series describes clinical features and outcomes in children with orbital inflammatory disease, with particular attention to recurrence, therapeutic approaches, and visual prognosis.
Methods: We retrospectively reviewed the medical records of 12 pediatric cases (ages 3–18 years; all female) with orbital inflammatory disease seen at Texas Children’s Hospital between October 2015 and June 2024. Data collected includes clinical presentation, laterality, lacrimal gland and optic nerve involvement, treatment regimens, recurrence, and outcomes. All patients underwent biopsy by an oculoplastic surgeon with histopathology reviewed with an ocular pathologist.
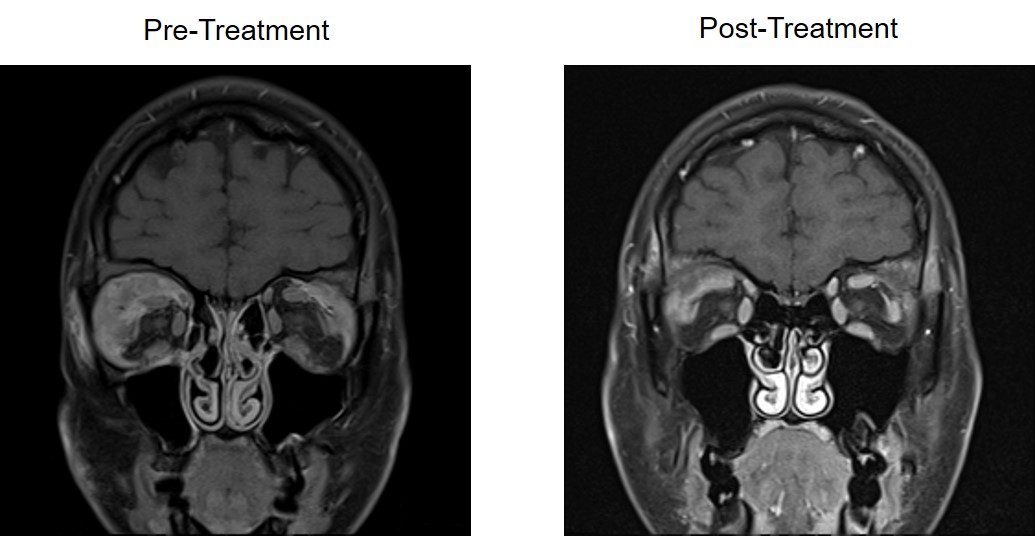
Results: The most common presenting symptoms were eyelid swelling (75%), proptosis (50%), ptosis (42%), and blurry vision (33%) (Table 1). The presenting symptoms were bilateral in 5 patients. Lacrimal gland involvement was common (75%), particularly in patients with ANCA vasculitis or IgG4-related disease. Optic nerve involvement was noted in 2 cases.Treatment regimens varied by diagnosis and response. Most ANCA-associated cases were managed with methotrexate and glucocorticoids, with escalation to rituximab, surgery, or additional immunosuppressant. Among these, 3 of 4 patients experienced disease recurrence, and one had progressive vision loss requiring a change in therapy. Patients with IgG4-related disease were primarily managed with rituximab or mycophenolate, with favorable outcomes and no recurrences reported (Figure 1).Nonspecific orbital inflammation (NSOI) cases demonstrated a heterogeneous response. Three of 4 patients required escalation beyond methotrexate and glucocorticoids, with rituximab leading to partial improvement in 2.Overall, recurrence occurred in 42% of cases predominantly in ANCA and NSOI diagnoses. Patients with IgG4-related disease did not require escalation of therapy.
Conclusion: Pediatric orbital inflammatory diseases exhibit diverse clinical presentations and outcomes. ANCA-associated orbital disease demonstrates a higher risk of recurrence and treatment escalation compared to IgG4-related disease. Of note, ANCA-associated vasculitis in pediatric patients did not manifest the bony sinonasal obliteration observed in adult patients. Lacrimal gland involvement is frequent; optic nerve compromise is rare. Rituximab appears effective across etiologies, particularly in refractory cases. This case series highlights the rarity of these diseases in children, importance of early recognition, and close longitudinal follow-up in managing these complex disorders.
.jpg) Figure 1. MRI Brain and Orbits Coronal T1 FS images showing bilateral inflammatory orbital masses pre- and post-treatment with rituximab and glucocorticoids in a patient with IgG4-related ocular disease.
Figure 1. MRI Brain and Orbits Coronal T1 FS images showing bilateral inflammatory orbital masses pre- and post-treatment with rituximab and glucocorticoids in a patient with IgG4-related ocular disease.
To cite this abstract in AMA style:
Elrefai R, Williams K, Bradfield H. Inflammatory Orbital Diseases: Pediatric Case Series From a Tertiary Care Center [abstract]. Arthritis Rheumatol. 2025; 77 (suppl 9). https://acrabstracts.org/abstract/inflammatory-orbital-diseases-pediatric-case-series-from-a-tertiary-care-center/. Accessed .« Back to ACR Convergence 2025
ACR Meeting Abstracts - https://acrabstracts.org/abstract/inflammatory-orbital-diseases-pediatric-case-series-from-a-tertiary-care-center/