Session Information
Session Type: Poster Session B
Session Time: 9:00AM-11:00AM
Background/Purpose: An increase in the incidence of autoimmune diseases after COVID-19 has been reported. Since many diseases exhibit population-specific causal effect sizes, we aimed to evaluate the incidence trends of inflammatory arthritis (IA), including rheumatoid arthritis (RA), after COVID-19 in a large admixed Colombian population.
Methods: Data analysis for this retrospective, population-based cohort study was carried out using the COOSALUD EPS registry. COOSALUD EPS is a health insurance company, belonging to the subsidized regime in Colombia. The registry includes demographic and epidemiological data on diagnoses identified during admission and defined by the International Classification of Diseases (ICD-10). The following codes were selected for analyses: M059, seropositive RA, defined by the presence of rheumatoid factor (RF) or anti-citrullinated protein antibody (ACPA); M069, unspecified RA, in which RF and ACPA were not confirmed; M060 seronegative RA, in which RF and ACPA were negative; and other RA-related diagnoses: M064, M139, M068, M058, M130 and M053. All the diagnosis were made by qualified rheumatologists. The study period was limited to January 01, 2020, through December 31, 2022. Incidence rates (IRs) and incidence rate ratios (IRRs) were assessed. IRRs were computed by comparing the IR of those who had COVID-19 prior to the IA diagnosis and those who did not have COVID-19 prior to the IA diagnosis. A Cox survival model was built to evaluate the influence of age, gender, and COVID-19 vaccination status on the development of IA.
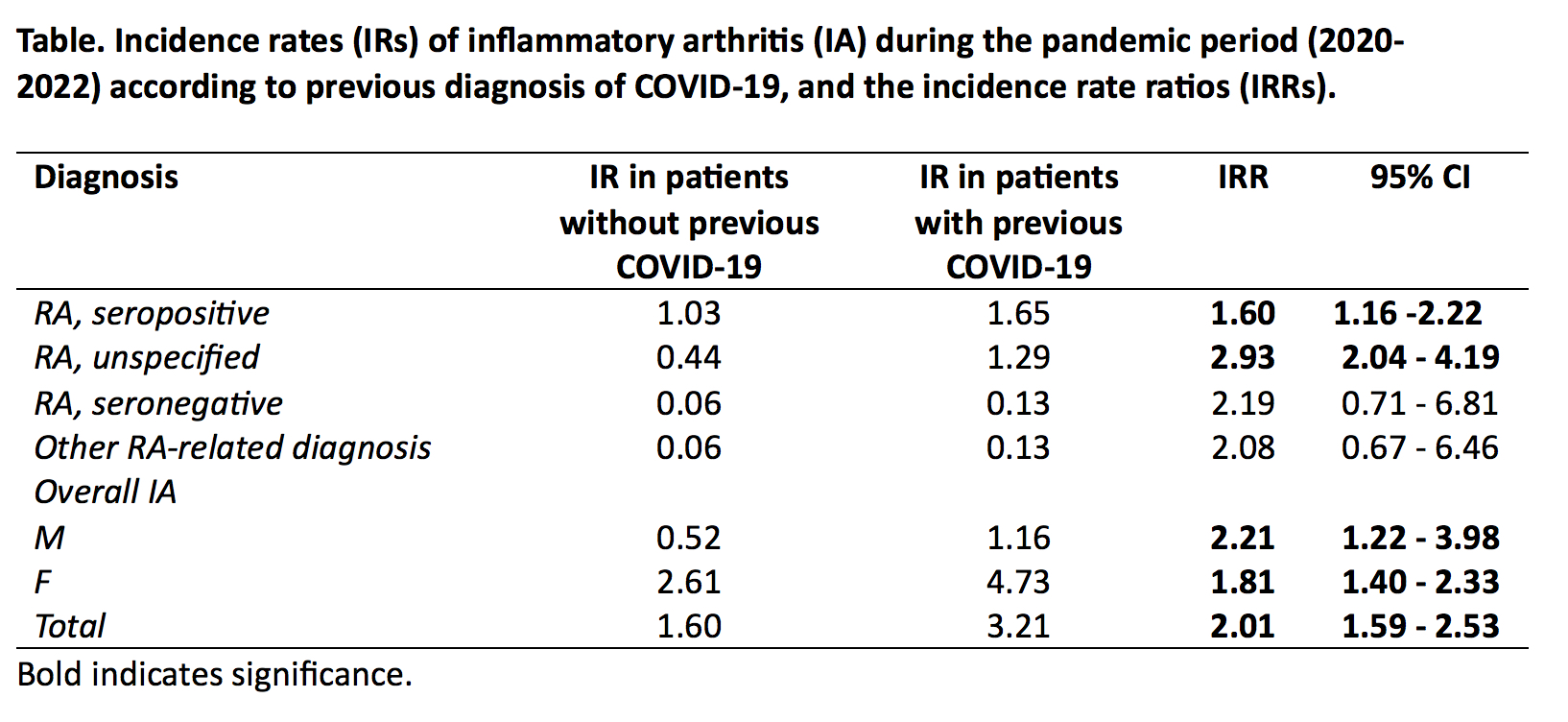
Results: The entire population study comprised 3,335,084 individuals, of whom 1,720,579 (51.59%) were women. The IRs of IA during the pandemic period (2020-2022) according to a previous diagnosis of COVID-19 and the respective IRRs are shown in the table. The associations remained significant after controlling for sex. The fitted Cox survival model showed that all the variables considered were significant (p< 0.05). The age groups estimates were increased until the age group of 51-60 years (HR: 9,163 95% CI: 7,245 – 11,589) and then decreased in the age group 61 years or older (HR: 5,364, 95% CI: 4,243 – 6,781) compared to those within 18-30 years. Men were less at risk than women to develop IA (HR: 0,2115, 95% CI: 0,182 – 0,246). The greater time since COVID-19 diagnosis was associated with a lower likelihood of developing IA (HR: 0,9986, 95% CI: 0,998 – 0,999). In vaccinated population, the probability of developing IA was reduced from HR: 3.345, 95% CI: 1.617 – 6.918 to HR: 3.232, 95% CI: 1.281 – 8.155 compared to those who did not have COVID-19. The model fitted well (Likelihood ratio test =2.074 p< 0,05; concordance = 0.77, p< 0,05).
Conclusion: Our findings indicate that the incidence of IA, including RA, increased following COVID-19, with the greatest increase occurring before the first year post-covid. Women were more susceptible than men. COVID-19 vaccination appears to be a protective factor.
To cite this abstract in AMA style:
Marin J, Mazenett E, Sarmiento M, Perez R, Morales C, Dominguez J, Salazar J, Anaya J. Increased Incidence of Inflammatory Arthritis After COVID-19 in a Colombian Population [abstract]. Arthritis Rheumatol. 2023; 75 (suppl 9). https://acrabstracts.org/abstract/increased-incidence-of-inflammatory-arthritis-after-covid-19-in-a-colombian-population/. Accessed .« Back to ACR Convergence 2023
ACR Meeting Abstracts - https://acrabstracts.org/abstract/increased-incidence-of-inflammatory-arthritis-after-covid-19-in-a-colombian-population/