Session Information
Date: Monday, November 18, 2024
Title: Muscle Biology, Myositis & Myopathies – Basic & Clinical Science Poster III
Session Type: Poster Session C
Session Time: 10:30AM-12:30PM
Background/Purpose: In inflammatory myopathies (IM), although several treatments effectively control disease activity, a high proportion of patients display sustained disability (damage). Damage might be reversed by intensive resistive exercise, but no pharmacological treatment is available. Moreover, damage assessment in daily clinical practice is an unmet need.
We previously showed, in a cohort of IM patients with no or low disease activity, that the decrease in the serum levels of two myokines, irisin and osteonectin, was associated with sarcopenia (decrease in appendicular muscle mass [ALM] and grip strength)1 and positively correlated with ALM and grip strength, respectively2. Moreover, ALM and grip strength were negatively associated with global damage, extent and severity damage scores according to IMACS2.
This study aimed to investigate the importance of myokine imbalance in IM disease damage.
Methods: Body composition by X-ray absorptiometry, functional tests, and serum levels of some myokines (irisin, osteonectin, fatty acid-binding proteins [FABP] and procollagen type III N-terminal peptide [PIIINP]) by ELISA were assessed at inclusion in forty adult IM patients (disease duration ≥12 months, low or no disease activity for ≥6 months) and thirty healthy age, sex and physical activity-matched volunteers (HV).
IM damage extent and severity in all domains, according to IMACS, were recorded. Overall rating of disease damage according to expert clinical judgement was also assigned to each patient (global damage) using a 10 cm visual analogue scale.
Relationships between the myokines serum levels and IMACS damage scores were determined using Pearson’s or Spearman’s rank test as appropriate. R is indicated in the text as correlation coefficient.
Results: Forty patients (27 females, 67.5%), mean age 59.9 (14.1) years were prospectively enrolled. Eight patients suffered from dermatomyositis (20%), 12 from necrotizing myopathy (30%), 11 from antisynthetase syndrome (28%), and 9 from scleromyositis (23%) from 4.6 years (2.9–8.4). At inclusion, physician global activity was 3/10 [2–3], CK 122 (87.5–195.5) U/l, MMT-8 140/150 (135.3–147) and MMT-12 213/220 (203.3–216.8).
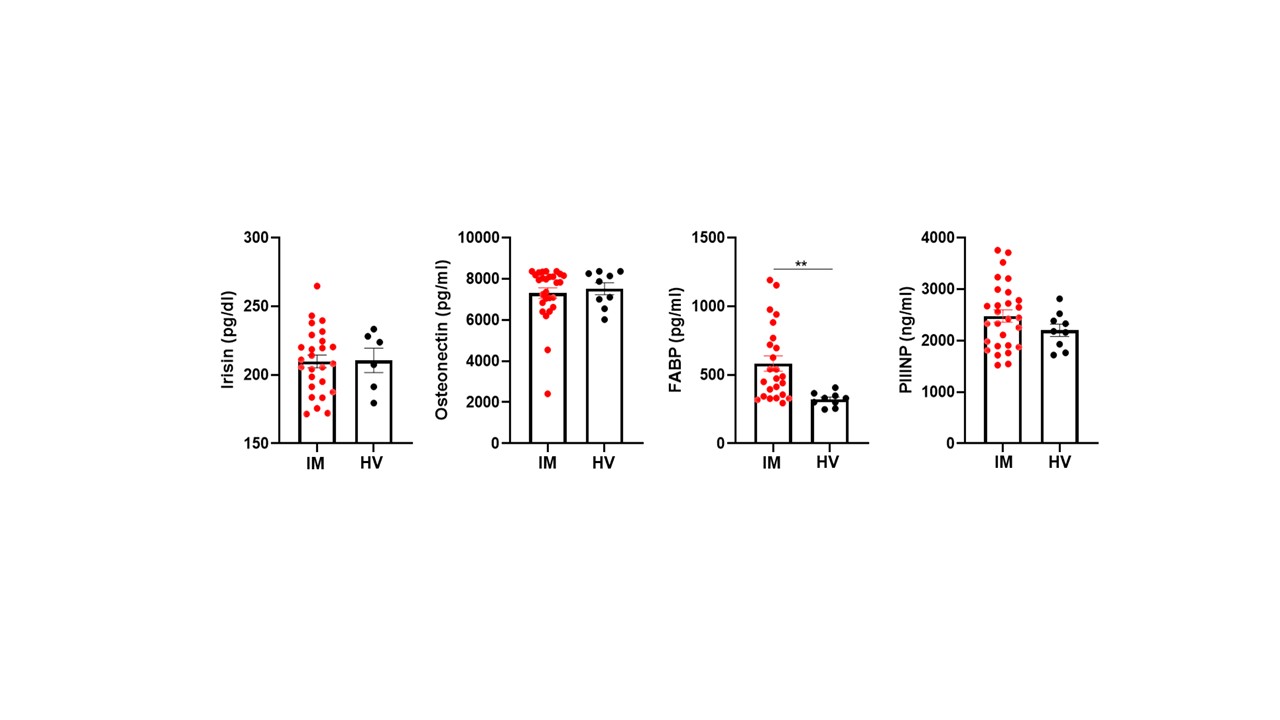
Irisin, osteonectin and PIIINP serum levels were similar in IM patients and HV, whereas FABP serum levels were higher in IM patients compared to HV (582.9 ± 273.2 vs. 320.3 ± 50.8 pg/ml, p= 0.001) (Figure 1). Moreover, FABP serum levels positively correlated with total damage extension (R= 0.5, p= 0.007), severity (R= 0.5, p= 0.006) and global damage score (R= 0.5, p= 0.01). Interestingly, FABP serum levels also positively correlated with gastrointestinal extension (R= 0.5, p= 0.02) and severity (R= 0.5, p= 0.02) damage score.
No significative correlation was found between FABP serum levels and body mass index and fat mass.
Conclusion: Increased circulating levels of FABP are candidate biomarkers of disease damage in IM similarly to that found in metabolic disorders3.
References
1Cruz-Jentoft AJ, et. Age Ageing. 2019 Jan 1;48(1):16-31. doi: 10.1093/ageing/afy169. Erratum in: Age Ageing. 2019 Jul 1;48(4):601.
2Giannini M, et al. Rheumatology (Oxford). 2024 Mar 27:keae207.
3Li B, et al. Cell. 2020 Aug 20;182(4):1066-1066.e1.
To cite this abstract in AMA style:
Giannini M, Charles A, Blaess J, Javier R, Geny B, Meyer A. Increased Circulating Levels of Fatty Acid-binding Proteins as a Potential Biomarker of Disease Damage in Inflammatory Myopathies Patients [abstract]. Arthritis Rheumatol. 2024; 76 (suppl 9). https://acrabstracts.org/abstract/increased-circulating-levels-of-fatty-acid-binding-proteins-as-a-potential-biomarker-of-disease-damage-in-inflammatory-myopathies-patients/. Accessed .« Back to ACR Convergence 2024
ACR Meeting Abstracts - https://acrabstracts.org/abstract/increased-circulating-levels-of-fatty-acid-binding-proteins-as-a-potential-biomarker-of-disease-damage-in-inflammatory-myopathies-patients/