Session Information
Session Type: Abstract Submissions (ACR)
Background/Purpose: miR-146a as an endogenous regulator plays a critical role in resolving acute inflammation. The risk-associated genetic variant in miR-146a promoter was linked to reduced expression of miR146a in the peripheral blood leukocytes of lupus patients. Our previous studies also showed that overexpression of miR-146a in PBMCs from patients with SLE suppressed coordinate activation of type I interferon (IFN) pathway. Pristane-induced lupus is a well established SLE murine model featuring abnormal activation of IFN pathway and unusual high penetrance of pulmonary capillaritis. This study explored a therapeutic potential of miR-146a in this induced murine model of lupus.
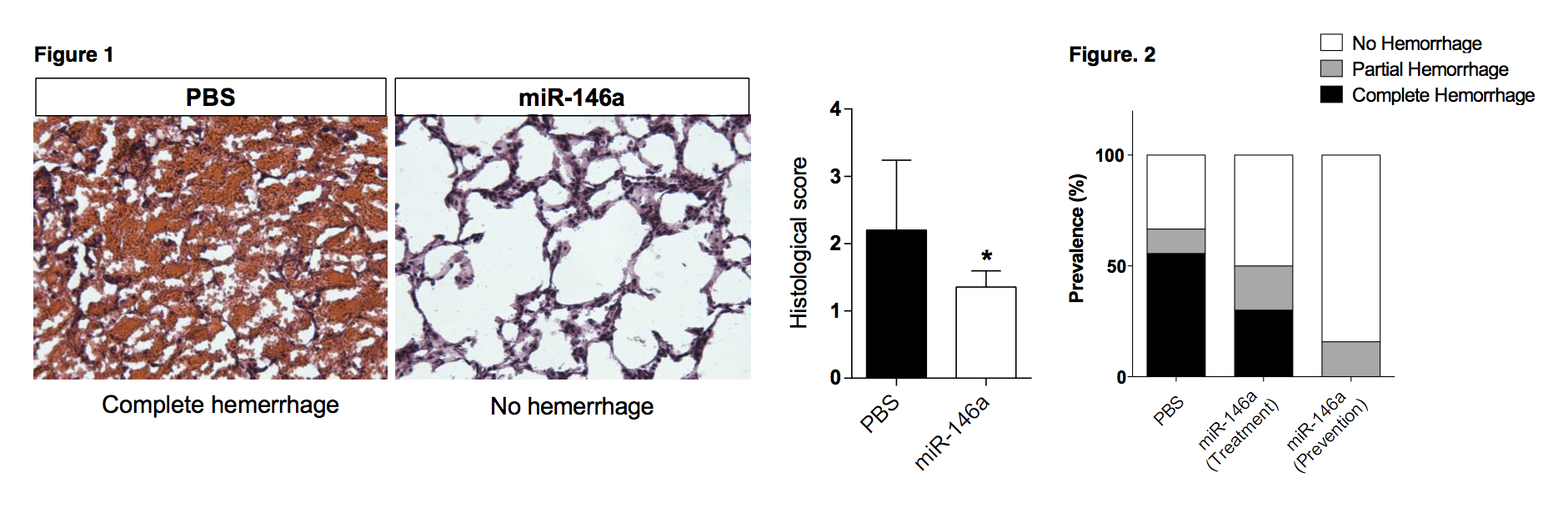
Methods: The C57BL/6 (B6) mice were intravenously injected with PBS or miR-146a via lateral tail veins. The peripheral bloods from 3, 7 and 14 days post Pristane injection were evaluated by real time PCR or gene expression profile analysis. For comparison, the B6 mice were categorized into 3 groups, receiving respectively 3 consecutive injections of PBS (control group, n=9) or miR-146a either 3 days before (prevention group, n =19) or 7 days after (treatment group, n=10) a single intraperiteneal injection of Pristane. The pulmonary hemorrhage was histologically investigated by HE staining 2 weeks post Pristane injection.
Results: The injections of miR-146a mimics (agomirs) resulted in a dramatic increase in the expression of peripheral blood miR-146a in both the prevention and treatment groups as compared to the control group receiving PBS. HE staining showed that miR-146a administration rendered mice resistant to Pristane-induced hemorrhagic pulmonary capillaritis (Fig. 1). While in the control group, 56% mice injected with Pristane developed complete pulmonary hemorrhage, the prevalence was reduced to 25% in the treatment group. Of note, the complete hemorrhage was completely blocked in prevention group (Fig. 2). Furthermore, qPCR revealed that miR-146a was significantly lower in mice with pulmonary hemorrhage compared with mice developing no hemorrhage (p < 0.01), and inversely correlated with expression of Mx1 (p < 0.01), an IFN-inducible gene. Gene expression profile analysis showed that miR-146a injection substantially suppressed the IFN response, accompanied by reduced production of multiple pro-inflammatory cytokines and chemokines.
Conclusion: Our study provides evidence that miR-146a plays a suppressive role in the Pristane-induced pulmonary hemorrhage in B6 mice. It also highlights a potential pathogenic role of type I IFN pathway activation in the development of pulmonary capillaritis in Pristane-induced murine lupus. These findings suggest that SLE patients with pulmonary hemorrhage may benefit from therapeutic intervention to induce miR-146a expression.
Disclosure:
D. Liang,
None;
S. Zhou,
None;
Z. Liu,
None;
Z. Shan,
None;
P. Brohawn,
None;
Y. Yao,
None;
J. B. Harley,
None;
N. Shen,
None.
« Back to 2013 ACR/ARHP Annual Meeting
ACR Meeting Abstracts - https://acrabstracts.org/abstract/in-vivo-administration-of-mir-146a-protects-c57bl6-mice-from-pristane-induced-pulmonary-hemorrhage-via-suppressing-type-i-interferon-response/