Session Information
Session Type: Poster Session C
Session Time: 1:00PM-3:00PM
Background/Purpose: We have documented that patients with rheumatoid arthritis (RA) are at increased risk to develop cardiovascular disease (CVD) compared to the general population, even after correction for traditional risk factors, a risk similar to that of patients with diabetes mellitus (DM). The objective of the current study was to extend our investigation to a follow up of more than 20 years, with a special focus on patients without prevalent CVD.
Methods: The CARRÉ study is an ongoing prospective cohort study on CV endpoints in 353 randomly selected patients with RA. Data was collected after three, ten, fifteen and twenty years of follow up. Results were compared to those of a reference cohort (n = 2484) enriched for type 2 DM. Primary focus was on patients without prevalent CVD at baseline. Hazard ratios for RA and DM patients compared to non-RA/-DM controls were calculated with cox proportional hazard models, and adjusted for baseline SCORE1 (a score that estimates 10-year risk of death due to CVD based on age, sex, smoking, systolic blood pressure and cholesterol levels).
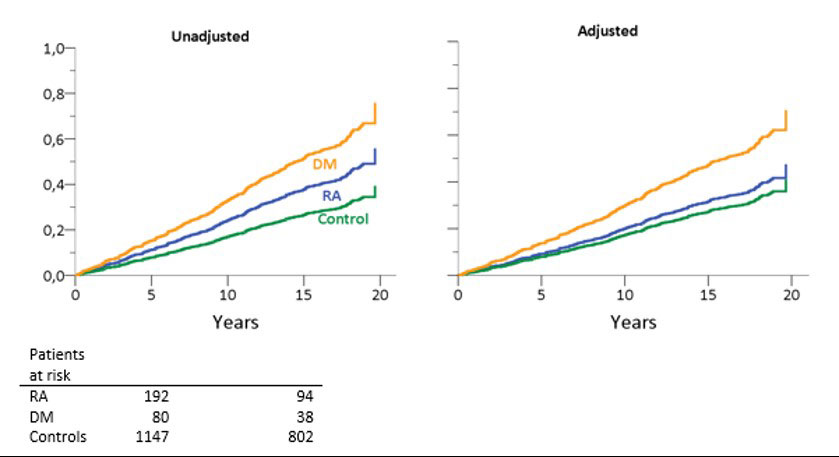
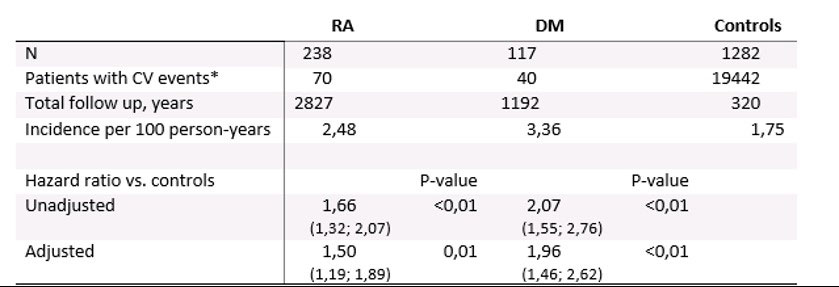
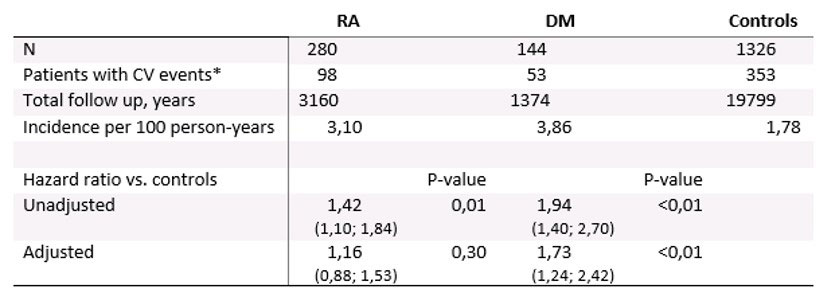
Results: 238 RA patients, 117 DM patients and 1282 controls, all without prevalent CVD at baseline were included in primary analyses. The primary analysis of events in patients without prevalent CVD shows that after adjustment for SCORE1, no relevant ‘RA-specific’ risk is observed, whereas a ‘DM-specific’ risk is retained (Table 1, Figure 1). In contrast, analyses of all cases (as was done in prior reports of this cohort) confirms the presence of an ‘RA-specific’ risk of about 50% (Table 2).
Conclusion: This new analysis of our cohort, now with 20-year follow up, focuses on CVD risk in RA patients without prevalent CVD, and was facilitated by the use of the SCORE1. These patients have an increased risk that is mainly attributable to increased presence of traditional risk factors. After adjustment for these factors, an increased risk attributable to RA only was thus preferentially seen in the patients with prevalent CVD at baseline. As RA treatment has improved over the observation period, this data suggests that the ‘RA-specific’ effect of inflammation preferentially targets damaged vessels. We suggest that with modern (early) treatment of RA, most of the increased CVD risk is mediated through traditional risk factors.
Right panel, hazard for rheumatoid arthritis (RA) and diabetes mellitus (DM) patients adjusted for
calculated SCORE1 results. Patients at risk shown are at the 5 and 15 year benchmarks.
* Both fatal and nonfatal events.
Hazard ratios are shown with 95% confidence intervals. Results were adjusted for calculated SCORE1 results. RA = rheumatoid arthritis, DM = diabetes mellitus, CV = cardiovascular.
* Both fatal and nonfatal events.
Hazard ratios are shown with 95% confidence intervals. Results were adjusted for calculated SCORE1 results. RA = rheumatoid arthritis, DM = diabetes mellitus, CV = cardiovascular.
To cite this abstract in AMA style:
Raadsen R, Agca R, Boers M, van Halm V, Peters M, Smulders Y, Beulens J, Blom M, Stehouwer C, Voskuyl A, Lems W, Nurmohamed M. In RA Patients Without Prevalent CVD, Incident CVD Is Only Associated with Traditional Risk Factors: A 20-year Follow up in the CARRÉ Cohort Study [abstract]. Arthritis Rheumatol. 2022; 74 (suppl 9). https://acrabstracts.org/abstract/in-ra-patients-without-prevalent-cvd-incident-cvd-is-only-associated-with-traditional-risk-factors-a-20-year-follow-up-in-the-carre-cohort-study/. Accessed .« Back to ACR Convergence 2022
ACR Meeting Abstracts - https://acrabstracts.org/abstract/in-ra-patients-without-prevalent-cvd-incident-cvd-is-only-associated-with-traditional-risk-factors-a-20-year-follow-up-in-the-carre-cohort-study/