Session Information
Date: Tuesday, November 14, 2023
Title: (1895–1912) Measures & Measurement of Healthcare Quality Poster II
Session Type: Poster Session C
Session Time: 9:00AM-11:00AM
Background/Purpose: Systemic sclerosis (SSc) is a complex autoimmune disease with significant morbidity and mortality. Quality indicators (QIs) for SSc care, previously published, are essential tools to enhance patient outcomes. However, a gap in the implementation of these QIs in clinical practice has been observed. This quality improvement project was designed to enhance the application of SSc QIs. The objectives of this study were to identify the quality gap in systemic sclerosis (SSc) care through assessment of recommended QIs and to evaluate the impact of targeted interventions to improve their uptake.
Methods: We conducted an interrupted time series study at 4 Scleroderma clinics across 2 hospitals over 10 months. Using the model for improvement framework, we employed the Plan-Do-Study-Act (PDSA) methodology to implement sequential change ideas. Interventions were increasing knowledge and awareness among physicians, implementing standardized care processes, and ensuring the availability of necessary devices. Outcome measures were the rates of completion of suboptimal baseline and monitoring/treatment QIs among newly diagnosed and early SSc patients. Process measures were the rates of SpO2 documentation, completion of annual pulmonary function tests (PFTs), baseline creatinine kinase (CK) measurements, blood pressure (BP) self-measurement counseling, and referrals to a hand exercise program for patients with reduced hand function. Balancing measures were staff satisfaction (5-point Likert scale, 1-5 from strong dissatisfaction to strong satisfaction) and perceived workload related to interventions (increase in time per patient).
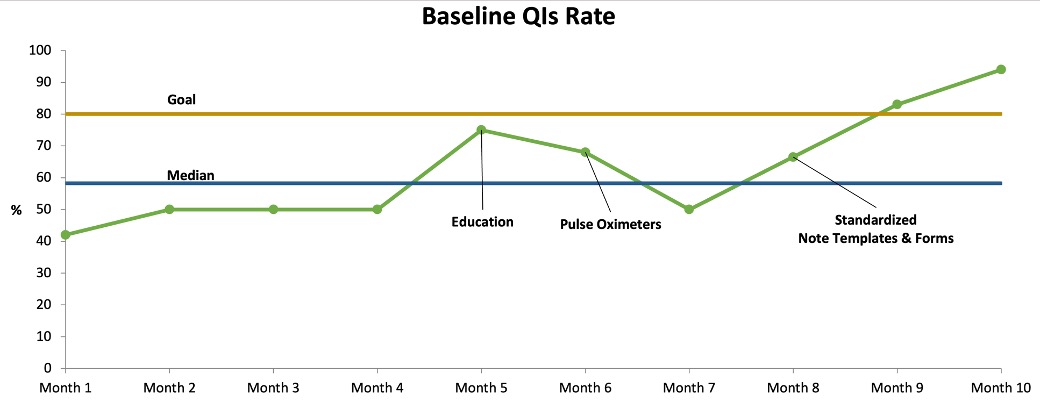
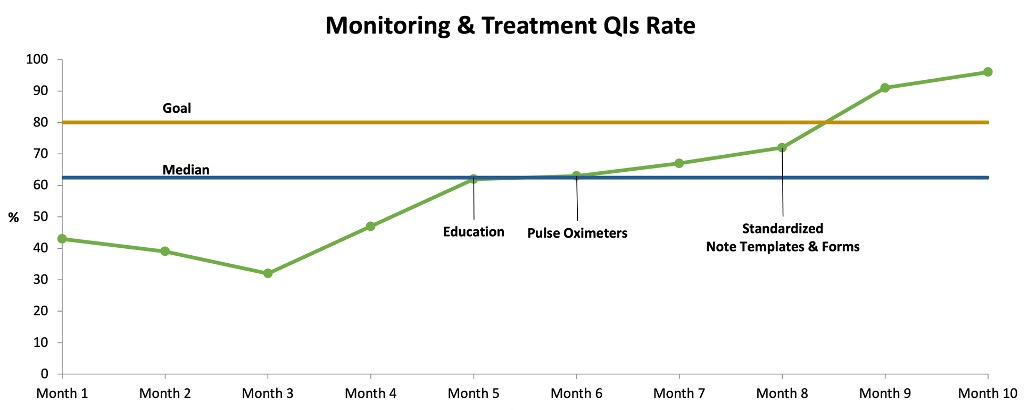
Results: The rate of baseline QIs among newly diagnosed SSc patients improved from 42% to 94% over 10 months (Figure. 1). The rate of monitoring and treatment QIs among early SSc patients improved from 43% to 96% (Figure. 2). Process measures including rates of SpO2 documentation during in-person visits (35.7% to 86%), completion of annual PFTs (64% to 100%), baseline CK measurements (33% to 100%), BP self-measurement counseling (0% to 100%), and referrals to a hand exercise program (33% to 100%) showed improvements. Balancing measures indicated stakeholder satisfaction (median rating 4) with the changes and no increased perceived workload (mean time increased by 2.5 minutes per patient).
Conclusion: The implementation of the interventions led to improvements in the rate of completion of QIs. Continuous monitoring through regular audits and the application of subsequent PDSA cycles as required is critical for sustaining these improvements. This initiative underscores the importance of systematic quality improvement in enhancing the management of complex autoimmune diseases like SSc.
To cite this abstract in AMA style:
Aboabat A, Aboulenain S, Ahmad Z, Soowamber M, Johnson S. In Pursuit of Excellence: Improving Systemic Sclerosis Quality of Care [abstract]. Arthritis Rheumatol. 2023; 75 (suppl 9). https://acrabstracts.org/abstract/in-pursuit-of-excellence-improving-systemic-sclerosis-quality-of-care/. Accessed .« Back to ACR Convergence 2023
ACR Meeting Abstracts - https://acrabstracts.org/abstract/in-pursuit-of-excellence-improving-systemic-sclerosis-quality-of-care/