Session Information
Session Type: Poster Session A
Session Time: 9:00AM-11:00AM
Background/Purpose: Herpes zoster (HZ), also known as shingles, causes an estimated one million cases annually in the United States. Many studies have shown that the risk for herpes zoster infection is higher in inflammatory rheumatic diseases (IRDs) and those who are immunocompromised (IC). The severity of herpes zoster correlates with underlying immunosuppression, also seen in immunosenescence. The rate of Shingles in our young IRD patients is similar to a healthy 65-year-old with a rate of 8-10 per thousand patient years. Some immunosuppressants (IS) especially JAKs further increase this risk.
Shingrix, approved in 2017 for adults over 50 years old, a non-live recombinant herpes zoster vaccine (RZV) is administered in two doses. In July 2021, the indication was expanded by the Federal Drug Association (FDA) to include patients eighteen years and older with IRDs or on IS. The purpose of our study was to study the prevalence of RZV in our young IRD cohort and to evaluate methods to increase vaccination rates, including utilization of the specialty pharmacy.
Methods: The patient cohort was collected utilizing the electronic medical record reporter system (EMRRS). All patients 18-49 years old who were seen in rheumatology clinic from July 2021 to mid-April 2022 were included to determine current RZV vaccination rates and eligibility. Eligibility criteria included young IRD patients and IC.
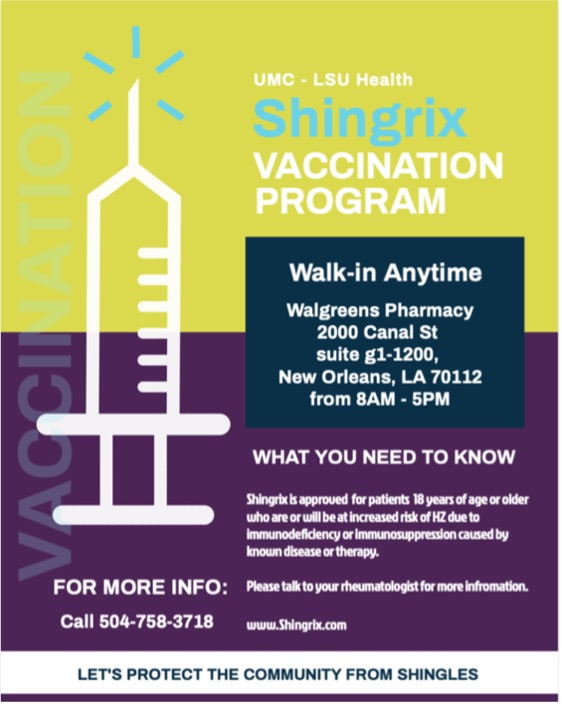
After determining which patients required RZV, the team coordinated with the specialty pharmacy to ensure a central location for inoculation and to keep a record of vaccinated patients. In addition, it ensured that patients would receive a reminder to return for the second dose of RZV. The pharmacists were provided with a list of eligible patients and the patients were given a flyer with pharmacy information. In addition, patients were electronically sent a copy of the flyer through the online patient portal or through email.
Cross-sectional analysis using EMRRS from July 2022 to June 1, 2023 was utilized by investigators to determine new eligible patients and the percentage of patients age 18-49 years old seen in rheumatology clinic that had received vaccination.
Results: A total of 1,009 patients ages 18-49 years old were seen in rheumatology clinic since the FDA expanded the indication for RZV. Of those patients, 458 were eligible to receive the vaccine. Prior to intervention, only two (0.2%) patients had received partial vaccination due to previous disseminated zoster infection. To date, 35.5% of eligible patients had been vaccinated, with 109 (23.8%) patients having received two doses of the vaccine and 58 (12.7%) patients having received the first vaccine dose. A majority of those receiving full vaccination were completed in the specialty pharmacy. The goal is to have 80% of eligible patients seen in rheumatology to be vaccinated.
Conclusion: RZV vaccination uptake has been markedly improved in our 18-49 years old eligible IRD patients, from 0.2% in April 2022 to 35.5% as of June 1, 2023. Even though the FDA may approve new guidelines, uptake is delayed, especially in the younger patient populations. The combination of multiple reminder avenues along with the coordination of specialty pharmacy proved successful in vaccinating eligible patients.
To cite this abstract in AMA style:
Lindsey S, Hill B, Sheth S, Loghmani A. Improving Vaccination Uptake of Herpes Zoster in Young Rheumatic Disease Patients Ages 18-49 Using Specialty Pharmacy Partnership [abstract]. Arthritis Rheumatol. 2023; 75 (suppl 9). https://acrabstracts.org/abstract/improving-vaccination-uptake-of-herpes-zoster-in-young-rheumatic-disease-patients-ages-18-49-using-specialty-pharmacy-partnership/. Accessed .« Back to ACR Convergence 2023
ACR Meeting Abstracts - https://acrabstracts.org/abstract/improving-vaccination-uptake-of-herpes-zoster-in-young-rheumatic-disease-patients-ages-18-49-using-specialty-pharmacy-partnership/