Session Information
Session Type: Poster Session C
Session Time: 1:00PM-3:00PM
Background/Purpose: The treat-to-target approach endorsed by the ACR for rheumatoid arthritis requires frequent monitoring of disease activity using validated instruments, with changes to the treatment regimen in order to target low disease activity or remission. The two university rheumatology clinics were using the Routine Assessment of Patient Index Data with 3 measures (RAPID-3) to measure disease activity. Historically, this had been given to the patient on paper at the time of an in-person clinic visit. Barriers to collecting RAPID-3 included; time taken at the beginning of the visit, incomplete form collection, manual entry into the electronic health record (EHR), and COVID-19 workflow changes resulting in gaps. We implemented electronic patient portal entry and point of care entry to address these barriers, with the goal of improving our collection rate.
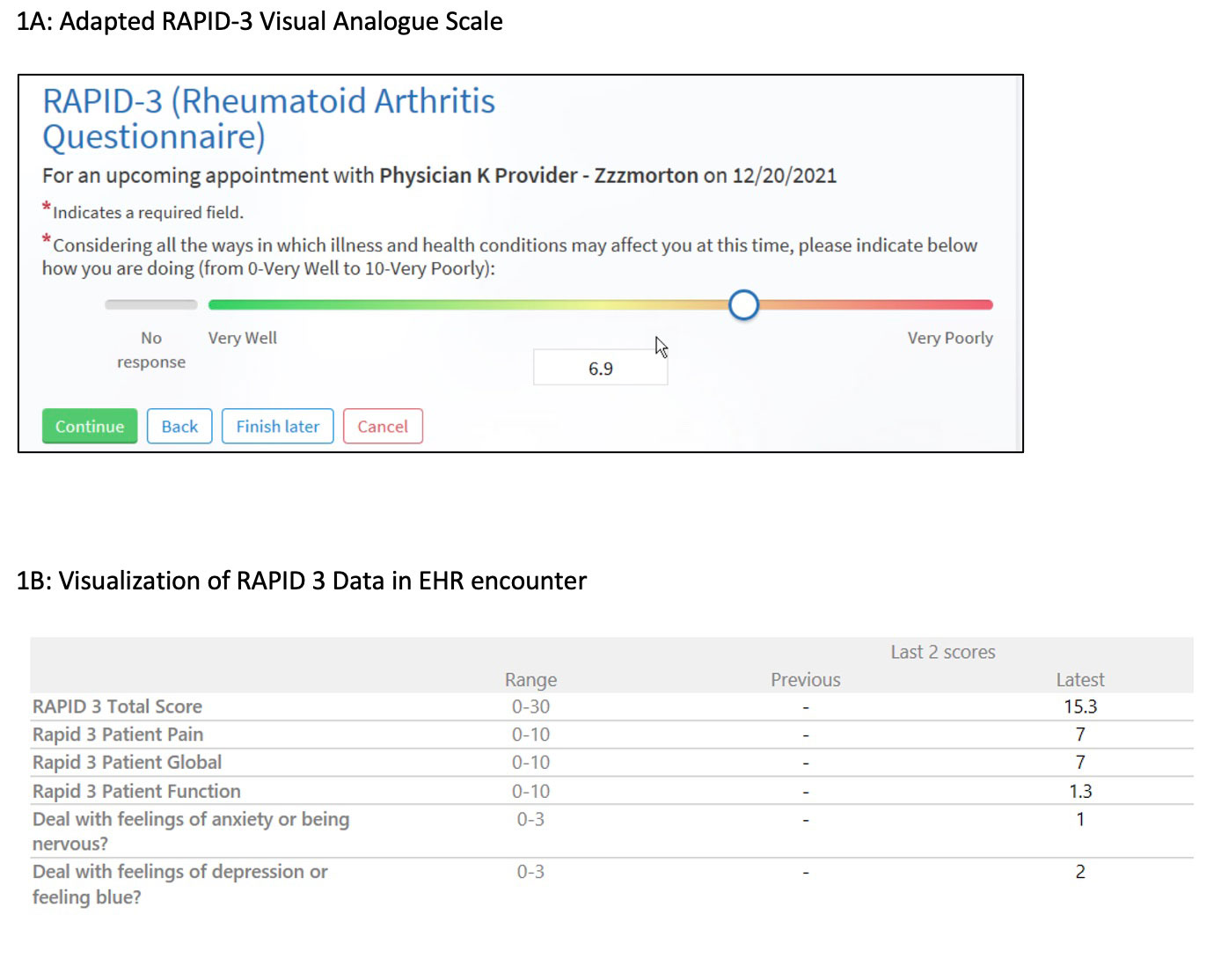
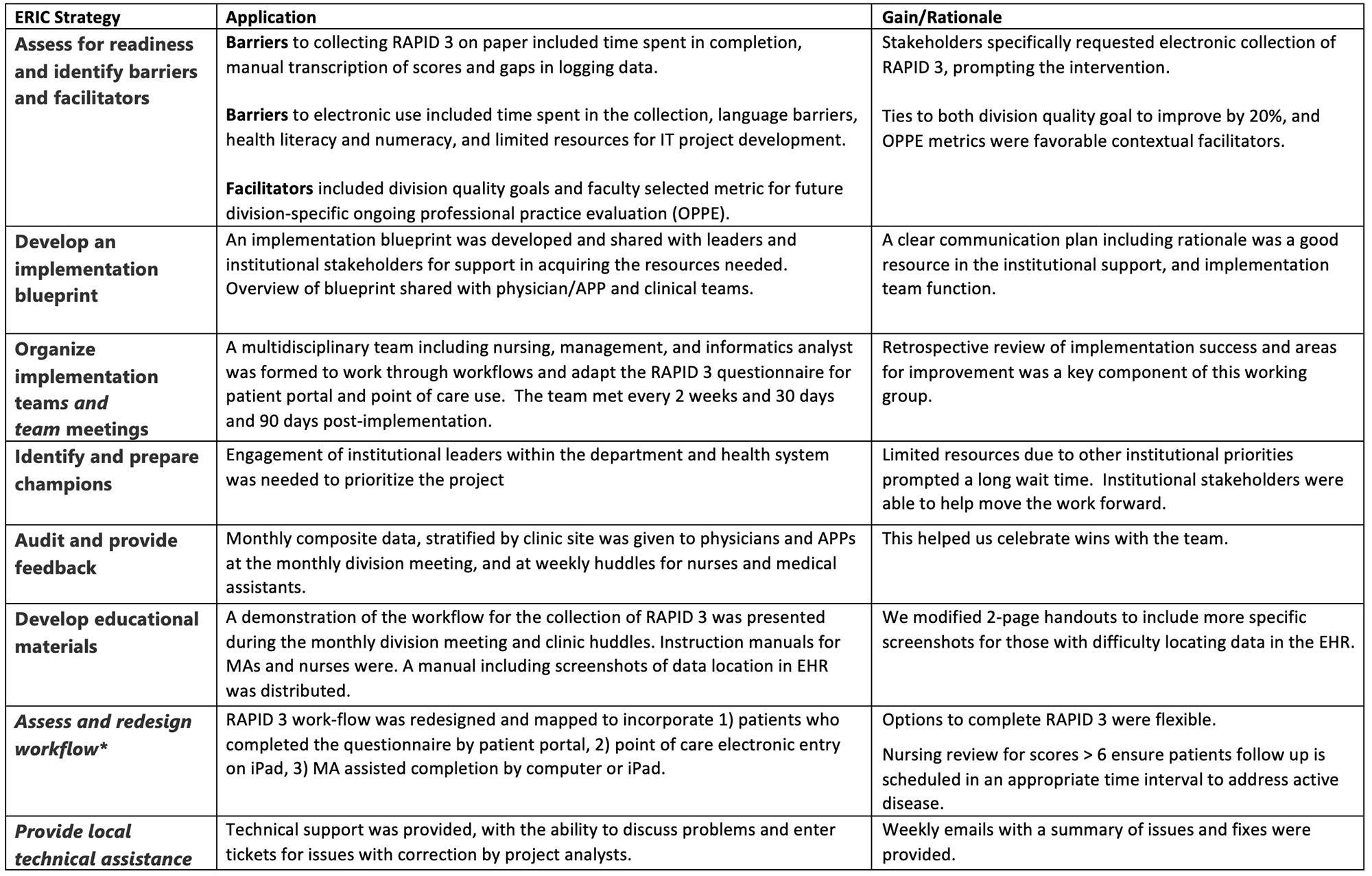
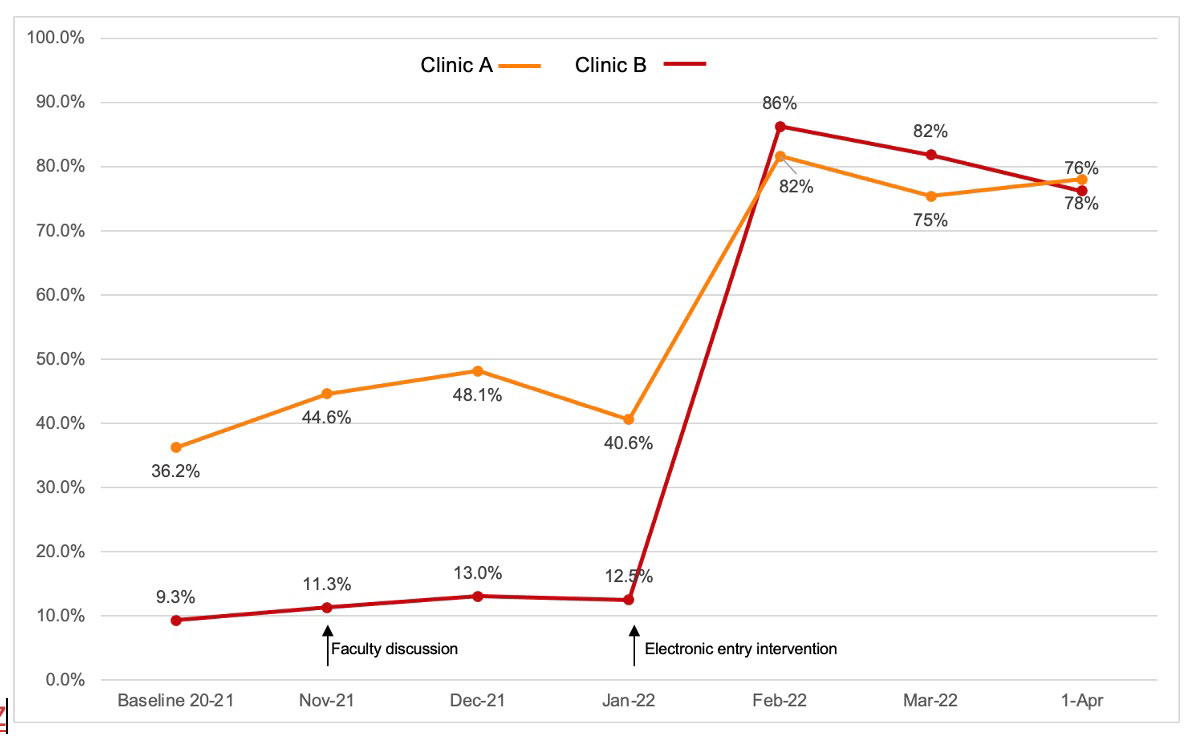
Methods: Baseline RAPID-3 data (7/2020 – 11/2021) were presented for patients with RA at both clinic sites prior to implementation during a monthly faculty meeting with a discussion of the importance of collecting disease activity measures. Barriers and facilitators to paper collection and future implementation of the patient portal and point of care electronic entry were discussed with faculty and in clinical support team huddles. Using the Consolidated Framework for Implementation Research (CFIR) Barrier Buster Tool (v0.52) we identified barriers that were mapped to Expert Recommendations for Implementing Change (ERIC) strategies to facilitate implementation (Table 1). A multidisciplinary team including physicians, nursing, and clinic leadership, and electronic health records analysts was formed to adapt the RAPID-3 tool for electronic patient portal use, and develop an implementation blueprint. The health IT converted paper tools into electronic items that were viewable on phones, tablets, and computer. This required adaptation of the visual analogue scale for phone (Fig 1A). Results are viewable within the encounter template (Fig 1B). Electronic tools went live 1/24/2022. Pre and 3-month post-implementation completion rates were compared using Fischer’s exact test.
Results: At baseline 36.2% of RA patient encounters at clinic site A and 9.3% at clinic site B had RAPID-3 scores entered (n = 317/875, 76/817; Fig 2 ). Following RAPID-3 faculty discussion, scores temporarily increased to 48.1% and 13% for sites A and B respectively. After patient portal and point of care electronic entry began, rates rose to 86% and 82%. Modest declines were noted afterwards with a 3-month average of 79.5% across all clinic encounters (n= 594/749, p < 0.001). For all patients who completed RAPID-3, 55.7% responded using the patient portal prior to visit.
Conclusion: Implementing electronic patient entered and point of care RAPID-3 assessments for RA significantly increased completion. Future efforts will include implementation strategies to support continued RAPID-3 collection and use in patient encounters.
To cite this abstract in AMA style:
Ferguson S, Zemlicka L, Weber A, Halabi A, Arnason J, Bartels C. Implementing RAPID-3 Using Electronic Patient Portal and Point of Care Entry [abstract]. Arthritis Rheumatol. 2022; 74 (suppl 9). https://acrabstracts.org/abstract/implementing-rapid-3-using-electronic-patient-portal-and-point-of-care-entry/. Accessed .« Back to ACR Convergence 2022
ACR Meeting Abstracts - https://acrabstracts.org/abstract/implementing-rapid-3-using-electronic-patient-portal-and-point-of-care-entry/