Session Information
Date: Tuesday, November 14, 2023
Title: (2039–2060) Pediatric Rheumatology – Clinical Poster III: Potpourri
Session Type: Poster Session C
Session Time: 9:00AM-11:00AM
Background/Purpose: Many pediatric patients are inadequately prepared for the transition from pediatric to adult subspecialty healthcare, and patients who fail to transition successfully are more vulnerable to poor health outcomes.Frequently, pediatric rheumatology clinics do not provide formal training or resources to develop skills related to this transition. Interventions to improve the transition process include implementing a transition policy andperiodically assessing patient and parent or caregiver readiness to transition.
Methods: A multidisciplinary transition team formed to improve processes related to transition to adult care by using quality improvement (QI) methodology. Beginning in July 2020, a modified Transition Readiness Assessment Questionnaire (TRAQ) was delivered through the electronic health record (EHR) for patients aged ≥ 14 years with ≥2 visits in the prior 3 years. Beginning in December 2021, questionnaires were automatically assigned annually during routine care. Questionnaires asked about patients’ interest in and perceived readiness for moving to an adult rheumatology setting by age 21, as well as need for education on skills required to navigate the medical system and advocate for one’s own needs. Questionnaires could be completed by either the patient or a parent or caregiver. Data was extracted via EHR reporting tools. QI methodology and descriptive statistics were used.
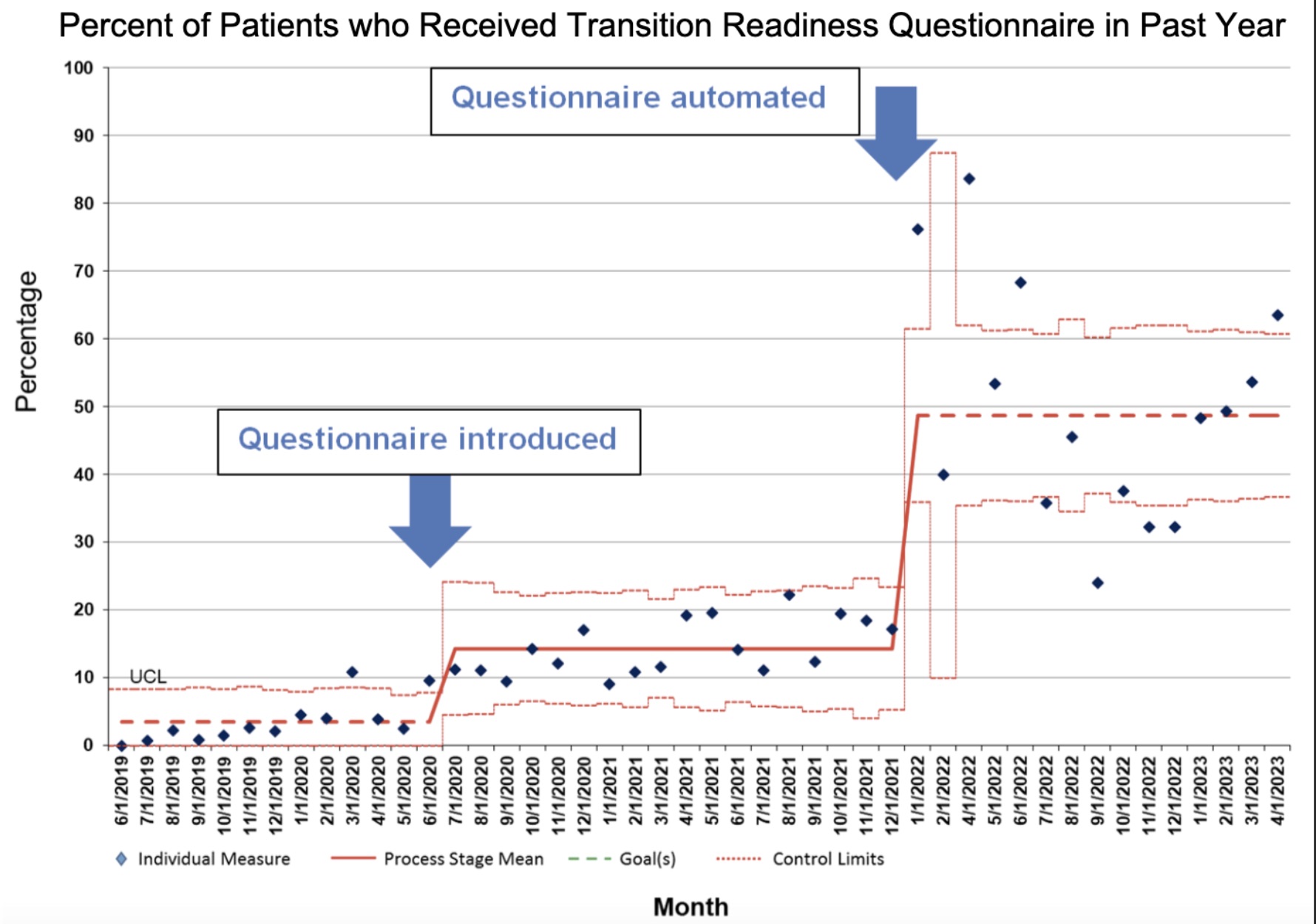
Results: Integrating automated questionnaires within the EHR significantly increased the proportion of patients aged ≥ 14 years who received a questionnaire from less than 20% to nearly 50% of patients (p< 0.001). This increase was sustained over the 16 months following the introduction of automated questionnaires (Figure 1).
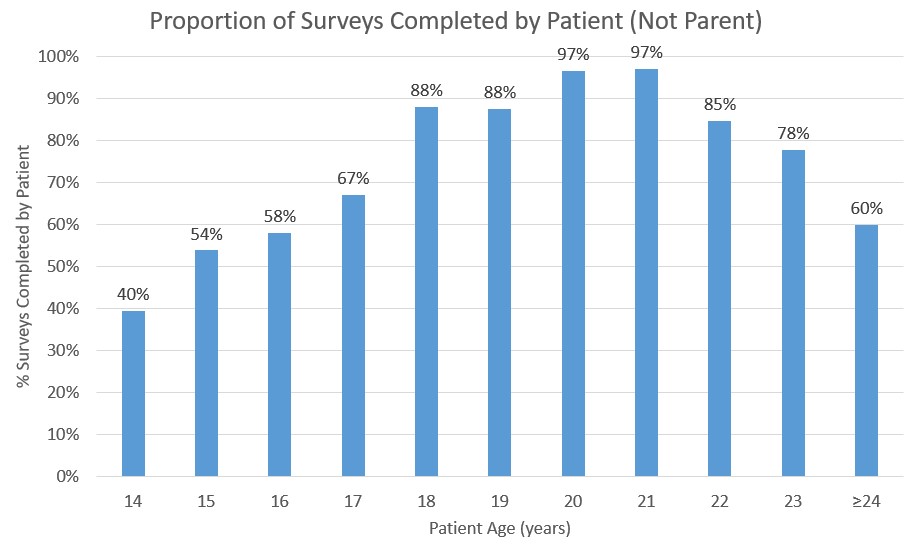
From January 2022 to April 2023, 1091 questionnaires were administered. Of these, 862 (79%) were fully completed and 918 (84%) had at least one question answered by 868 unique patients. The median age was 16 years [interquartile range 15, 18]. Fewer than half of 14-year-old patients completed the questionnaire themselves; the patient completion rate increased up to age 20-21, then decreased (Figure 2).
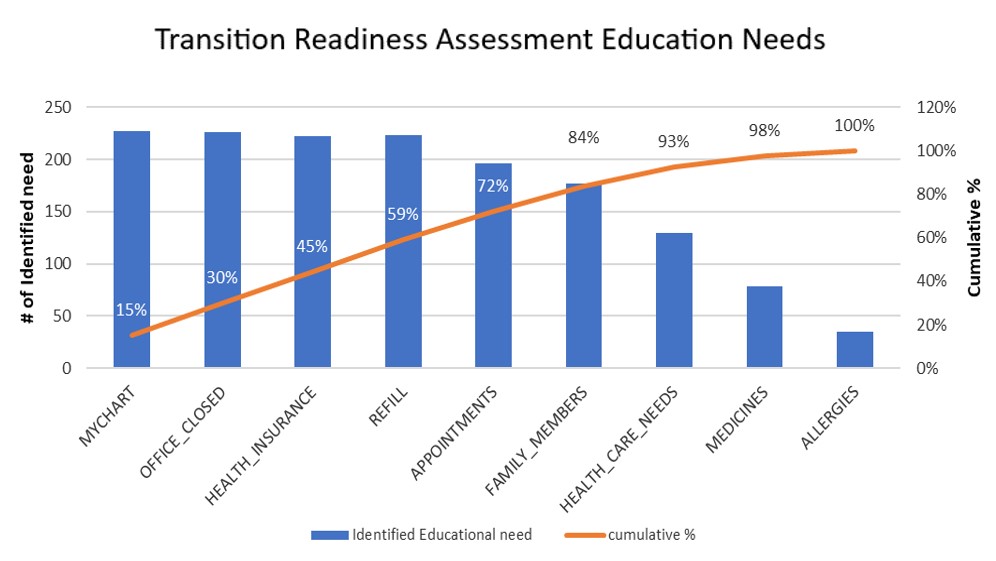
The most frequently identified educational needs related to EHR messaging, obtaining care if the office is closed, health insurance, refilling medications, making appointments, and awareness of family history. Together, these six factors accounted for over 80% of the identified needs (Figure 3).
Unsurprisingly, older patients reported less need for education on each skill assessed. Patients aged 14-17 were about twice as likely to report they could not complete each skill independently.
Conclusion: Integrating a transition readiness assessment in the EHR is feasible and can identify population-wide knowledge gaps as well as facilitate targeted individual education. In our population, the most perceived educational needs include EHR messaging, emergency care, health insurance, and refilling medications. Older patients are generally more likely to report competence at each skill assessed. This process can be implemented at other sites to help streamline transition readiness assessment and increase response rates.
To cite this abstract in AMA style:
Murray E, Argraves M, Taxter A, Wise K, Jensen P, Goldstein-Leever A, Thomas B, Scott A, Hughes J, Gallup J, Sumano Vicente D, Ardoin S, Sivaraman V. Implementation of an Automated Transition Readiness Assessment in a Pediatric Rheumatology Clinic [abstract]. Arthritis Rheumatol. 2023; 75 (suppl 9). https://acrabstracts.org/abstract/implementation-of-an-automated-transition-readiness-assessment-in-a-pediatric-rheumatology-clinic/. Accessed .« Back to ACR Convergence 2023
ACR Meeting Abstracts - https://acrabstracts.org/abstract/implementation-of-an-automated-transition-readiness-assessment-in-a-pediatric-rheumatology-clinic/