Session Information
Session Type: Poster Session A
Session Time: 1:00PM-3:00PM
Background/Purpose: The primary target for the treatment of rheumatoid arthritis (RA) is achieving remission or low disease activity with proper use of DMARD. Besides controlling disease activity, several poor prognostic factors (PPF) have been suggested by the ACR and the EULAR guidelines. However, the real-world data on clinical impacts of these PPF are limited. Our study aimed to elucidate differences in clinical characteristics, clinical outcomes, and biologic/targeted synthetic DMARD (b/tsDMARD) use according to the number of PPF in a large Korean cohort of patients with RA.
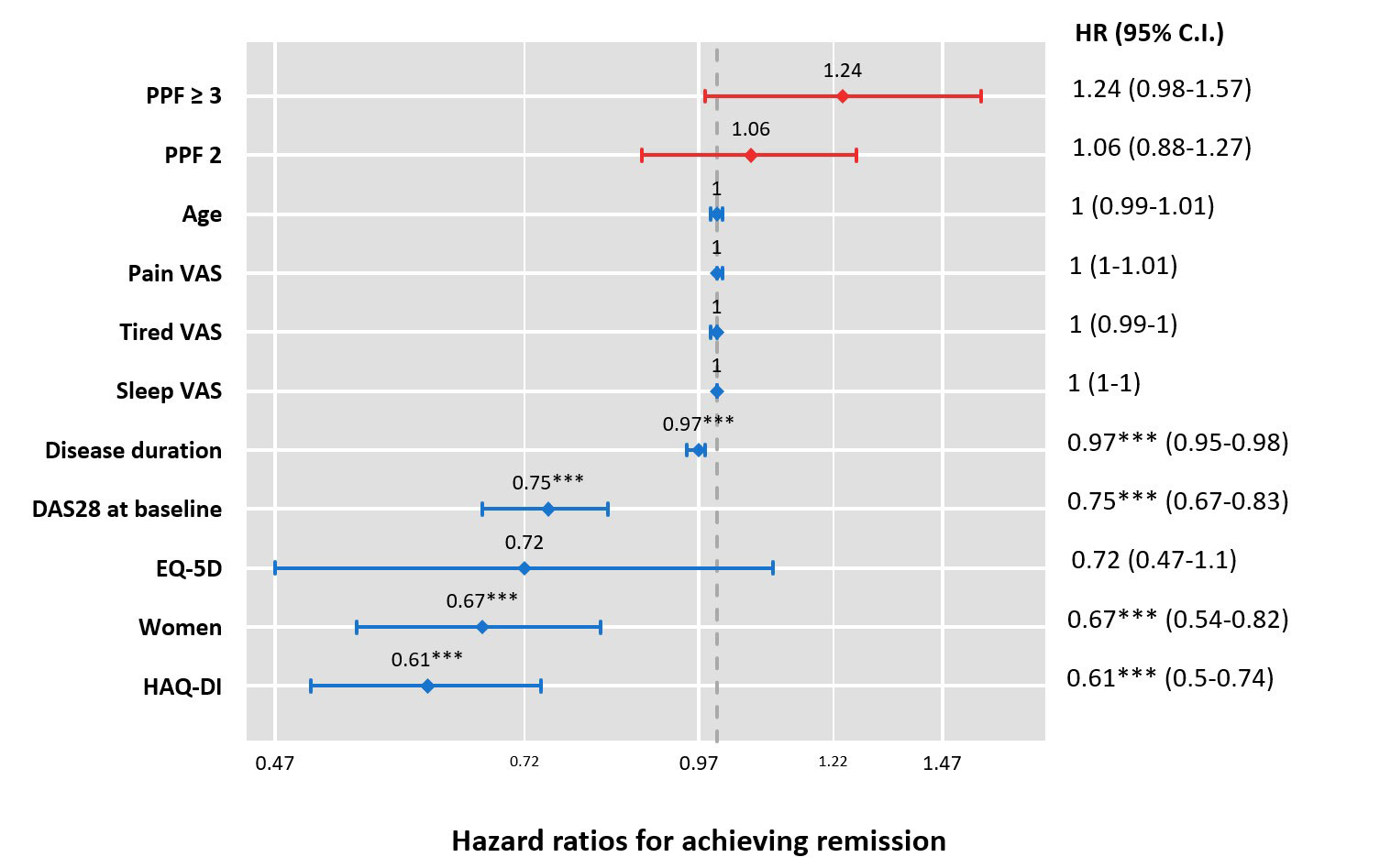
Methods: Using the KORean Observational study Network for Arthritis (KORONA) database, patients with RA were categorized by three groups having 0–1, 2, ≥ 3 PPF; functional limitation (HAQ-DI >0.5), extra-articular disease (Sjögren syndrome, RA lung disease, and/or nodules), seropositivity, and the presence of bone erosions. Baseline characteristics, comorbidities, and longitudinal changes of disease activity and patient-reported outcomes (PROs) were compared by PPF groups. Cox-proportional hazard regression analyses were used to evaluate the factors related to achieving clinical remission during follow-up within a subgroup with active disease at baseline and risks for the initiation of b/tsDMARD among biologic-naïve RA patients at baseline.
Results: A total of 5,077 patients with RA were included: 1,789 (35.2%), 2,027 (39.9%), and 1,261 (24.9%) had 0–1, 2, ≥ 3 PPF, respectively. The group with ≥3 PPF were older, more likely to be seropositive, and had longer RA disease duration than groups with low numbers of PPF. Moreover, the ≥3 PPF group exhibited higher disease activity (DAS28 4.43 ± 1.30, 3.79 ± 1.35, and 3.13 ± 1.18 in ≥3, 2, 0–1 PPF groups, respectively, p < 0.001) and patient-reported visual analogue scale (VAS) scores for global assessment, fatigue, and sleep disturbance and these trends were maintained during the 5-year follow-up period. Hypertension, diabetes mellitus, and congestive heart failure were more prevalent in ≥3 PPF group. Among 2,928 patients with active disease (DAS28 ≥3.2) at baseline, associated factors for achieving remission were male gender, low DAS28, and short disease duration. The ≥3 PPF group tended to be less likely to achieve remission, although statistically insignificant (adjusted HR [aHR] 1.24, 95% CI 0.98-1.57, p=0.07). More b/tsDMARD-naïve patients were initiated b/tsDMARDs during follow-up in ≥3 PPF (aHR 2.83, 95% CI1.79-4.46) and 2 PPF (aHR 1.88, 95% CI 1.23-2.86) compared with 0–1 PPF group.
Conclusion: RA patients with a greater number of PPF demonstrated higher disease activity and poorer PROs as well as worse longitudinal clinical outcomes. A higher number of PPF significantly predicted the clinician’s decision for b/tsDMARDs use. In addition to RA disease activity, the number of PPF should still be incorporated into the management of RA.
To cite this abstract in AMA style:
Ha Y, Shin S, CHOI S, Kang E, Lee Y. Impacts of Poor Prognostic Factors in Rheumatoid Arthritis on Clinical Outcomes and Treatment Choices from an Observational Cohort of Korean Patients with Rheumatoid Arthritis [abstract]. Arthritis Rheumatol. 2022; 74 (suppl 9). https://acrabstracts.org/abstract/impacts-of-poor-prognostic-factors-in-rheumatoid-arthritis-on-clinical-outcomes-and-treatment-choices-from-an-observational-cohort-of-korean-patients-with-rheumatoid-arthritis/. Accessed .« Back to ACR Convergence 2022
ACR Meeting Abstracts - https://acrabstracts.org/abstract/impacts-of-poor-prognostic-factors-in-rheumatoid-arthritis-on-clinical-outcomes-and-treatment-choices-from-an-observational-cohort-of-korean-patients-with-rheumatoid-arthritis/