Session Information
Date: Monday, November 9, 2020
Title: Pediatric Rheumatology – Clinical Poster III: SLE, Vasculitis, & JDM
Session Type: Poster Session D
Session Time: 9:00AM-11:00AM
Background/Purpose: Children with rheumatic diseases face unknown risks in the setting of the COVID-19 pandemic. These children are often immunosuppressed due to their underlying disease or the medications used to treat them. It is unknown whether children with rheumatic diseases are at increased risk of SARS CoV-2 infection or of developing serious disease complications should they become infected. We report on the pediatric data from the COVID-19 Global Rheumatology Alliance (C19-GRA) Patient Experience Survey.
Methods: The C19-GRA launched an international Patient Experience Survey for adults and parents of children with rheumatic disease, with or without COVID-19 infection. The survey was distributed online through patient support organizations and on social media. Parents completed the data on behalf of their children, including their child’s rheumatic disease diagnosis, medications, disease activity (as measured by a visual analog scale from 0-10, where 0=very good and 10=very poor), whether or not they developed COVID-19, and COVID-19 disease outcomes. Parents also completed the PROMIS Parent Proxy Scale v1.0 – Global Health 7. We report on data for children less than 18 years of age from April 3-May 8, 2020.
Results: A total of 427 children are included in the analyses. Their demographics and clinical characteristics are shown in Table 1. Most respondents resided in the Americas (64.9%) and were white (73.3%), female (63.0%), and between the ages of 5-14 (64.9%). The majority of patients had juvenile idiopathic arthritis, and most were taking conventional synthetic DMARDs (csDMARDs) and/or biologic DMARDs (bDMARDs). The median disease activity score was 3 (IQR 1-6). The median T-score of the PROMIS Global Health measure was 43.9. Within this group, only 5 children (1.2%) were diagnosed with COVID-19, and none required hospitalization. Their COVID-19 disease experience is shown in Table 2.
Conclusion: In this international survey of children with rheumatic diseases, only a handful of children developed COVID-19, all of whom had benign outcomes. Similar to otherwise healthy children, those with rheumatic disease do not seem to be at greater risk of developing COVID-19 or of COVID-19-related complications, even while taking immunosuppressive medications. Limitations of this study include a convenience sample of parents engaged in social media, which may not be representative of the pediatric rheumatology population. Data were self-reported and could not be verified. Future studies should assess the long-term effect of COVID-19 infection in patients with rheumatic disease, as well as assess the rates of complications such as Multisystem Inflammatory Syndrome in Children (MIS-C).
Disclaimer: The views expressed here are those of the authors and participating members of the COVID-19 Global Rheumatology Alliance and do not necessarily represent the views of the American College of Rheumatology, the European League Against Rheumatism (EULAR), or any other organization.
 Table 1. Demographic and clinical characteristics of children in the C19-GRA Patient Experience Survey (n=427).
Table 1. Demographic and clinical characteristics of children in the C19-GRA Patient Experience Survey (n=427).
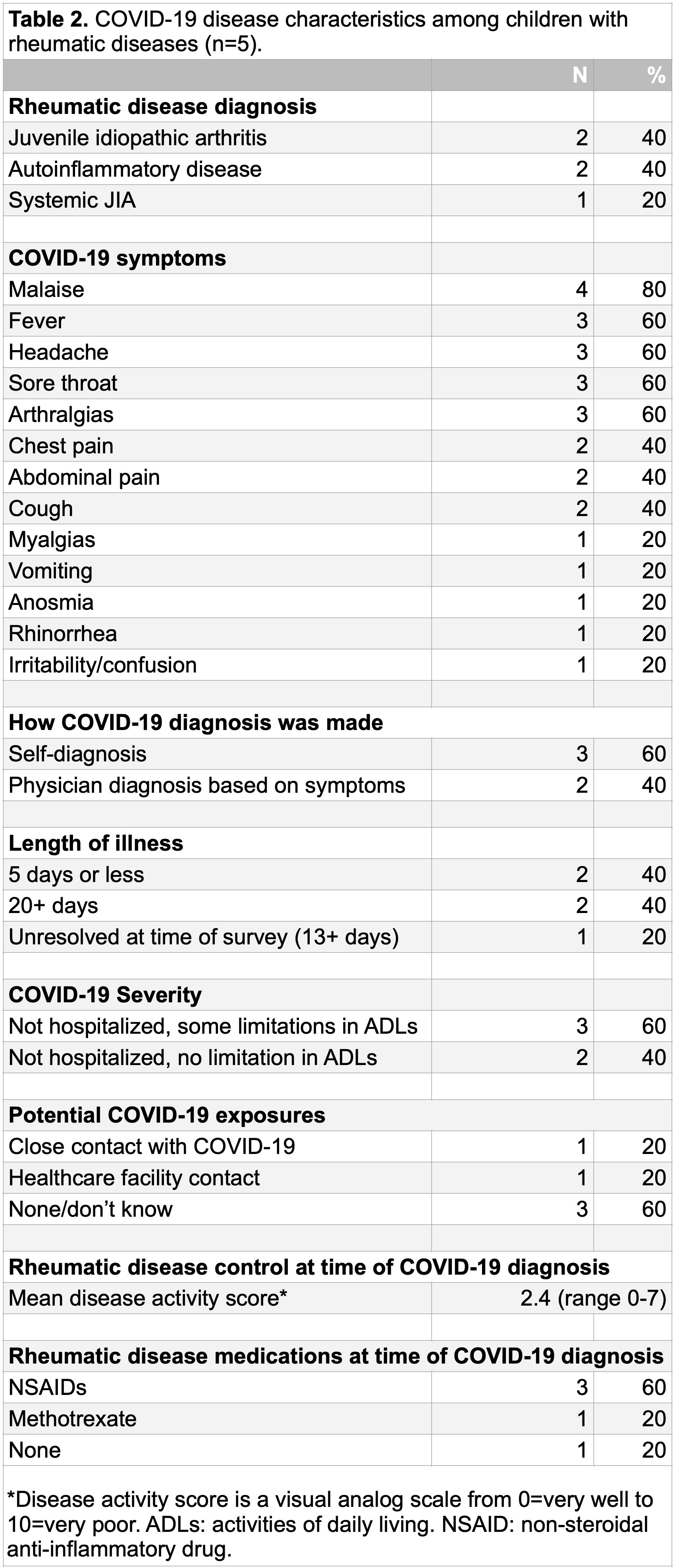 Table 2. COVID-19 disease characteristics among children with rheumatic diseases (n=5).
Table 2. COVID-19 disease characteristics among children with rheumatic diseases (n=5).
To cite this abstract in AMA style:
Hausmann J, Kennedy K, Surangiwala S, Larche M, Durrant K, Sinha R, Sirotich E. Impact of the COVID-19 Pandemic Among Children with Rheumatic Diseases from Around the Globe [abstract]. Arthritis Rheumatol. 2020; 72 (suppl 10). https://acrabstracts.org/abstract/impact-of-the-covid-19-pandemic-among-children-with-rheumatic-diseases-from-around-the-globe/. Accessed .« Back to ACR Convergence 2020
ACR Meeting Abstracts - https://acrabstracts.org/abstract/impact-of-the-covid-19-pandemic-among-children-with-rheumatic-diseases-from-around-the-globe/
