Session Information
Session Type: Abstract Session
Session Time: 3:00PM-4:30PM
Background/Purpose: When uncontrolled, JIA is associated with short-term and long-term complications that affect the patient’s quality of life. A common goal of treatment is to achieve clinically inactive disease (CID) status. The impact of insurance type on treatment initiation, biologic disease-modifying antirheumatic drugs (bDMARDs), for newly diagnosed JIA patients which may affect time to achieving CID has not been well established. The objective of this study was to investigate the importance of the health insurance type on bDMARD initiation and achievement of CID in patients with JIA.
Methods: De-identified data from all pediatric Rheumatology patients newly diagnosed with JIA between 2009 and 2020 at Cincinnati Children’s Hospital Medical Center were included in the study. JIA subtypes were defined as per the International League of Associations for Rheumatology (ILAR) classification codes. Outcome variables assessed included time from JIA diagnosis to bDMARD initiation and time to CID stratified by insurance type, public or private. The clinical Juvenile Arthritis Disease Activity Score (cJADAS) and Physician’s Global Assessment (PGA) were used to evaluate disease activity. Descriptive and survival statistics were utilized with a p < 0.05 indicating statistical significance.
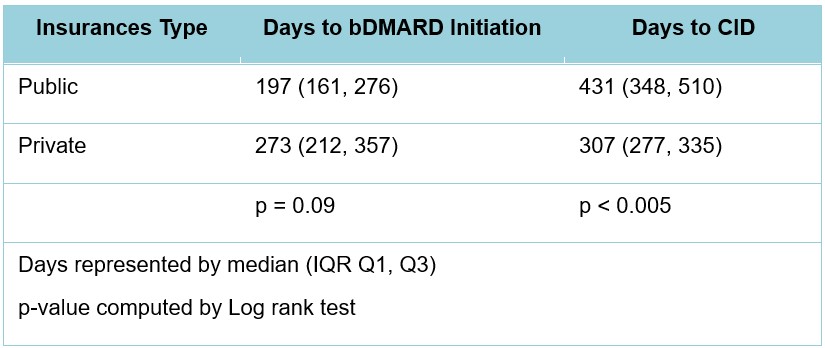
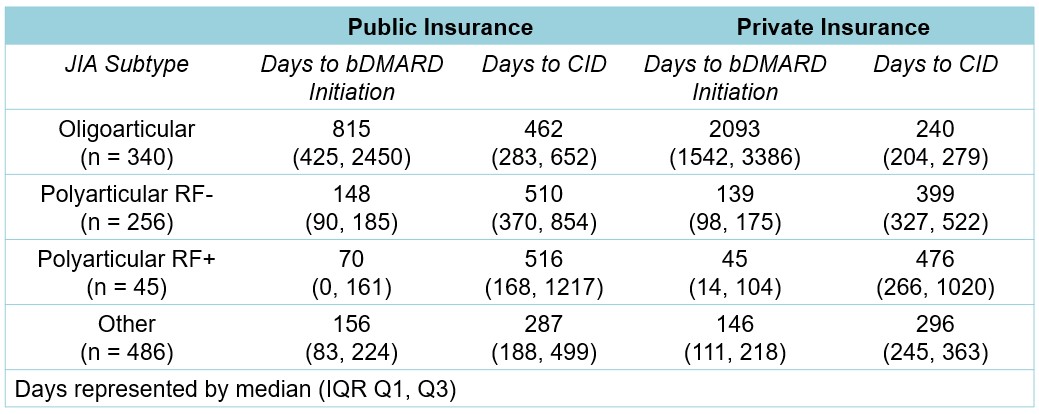
Results: A total of 1127 patients were newly diagnosed with JIA during the study period; of whom 835 (74.1%) patients were privately insured and 292 (25.9%) patients had public insurance. During the study there were 679 (60.3%) patients who initiated bDMARD therapy and 298 (26.4%) patients achieved CID. The cohort was comprised predominantly of patients of white or Caucasian (88.5%) race, with JIA subtypes classified as polyarticular (n=301, 26.7%), oligoarticular (n=340, 30.2%) and other (n=486, 43.1%). Significant differences between insurance types and race (p < 0.001) and age at time of JIA diagnosis (p=0.012) were observed. Patients with public insurance compared to private insurance were started significantly earlier post diagnosis on bDMARD therapy (197 days vs 273 days; p=0.09), but required significantly longer times to achieving CID (431 days vs 307 days; p < 0.005). Patients diagnosed with oligoarticular JIA who required bDMARDs received them significantly earlier when through public insurance compared to those with private insurance (815 days vs 2093 days; p < 0.05). However, the time to achieve CID was significantly shorter in patients with oligoarticular JIA on private compared to public insurance (240 days vs 462 days, p < 0.05).
Conclusion: This study supports our hypothesis that public insurance provided bDMARDs in a timelier fashion than private insurance. Further studies are required to understand reasons for the large variation of bDMARD initiation in oligoarticular JIA patients with public and private. Next steps include elucidating other barriers besides bDMARD access that limit the achievement of CID, especially in publicly insured children.
To cite this abstract in AMA style:
Yung E, Liu X, Huang B, Wagner M, Aundhia M, Chen C, brunner h. Impact of Insurance on Time to Biological Drug (bDMARD) Initiation and Inactive Disease Achievement in Patients with Juvenile Idiopathic Arthritis [abstract]. Arthritis Rheumatol. 2024; 76 (suppl 9). https://acrabstracts.org/abstract/impact-of-insurance-on-time-to-biological-drug-bdmard-initiation-and-inactive-disease-achievement-in-patients-with-juvenile-idiopathic-arthritis/. Accessed .« Back to ACR Convergence 2024
ACR Meeting Abstracts - https://acrabstracts.org/abstract/impact-of-insurance-on-time-to-biological-drug-bdmard-initiation-and-inactive-disease-achievement-in-patients-with-juvenile-idiopathic-arthritis/