Session Information
Date: Monday, November 13, 2023
Title: (1264–1307) RA – Diagnosis, Manifestations, and Outcomes Poster II
Session Type: Poster Session B
Session Time: 9:00AM-11:00AM
Background/Purpose: Tender and swollen joints counts may be differentially affected in rheumatoid arthritis (RA) patients with obesity. A prior study demonstrated an association between increased BMI and swelling of the lower extremity joints (Ranganath et al. 2019). To our knowledge, there are no publications describing the impact BMI has on musculoskeletal ultrasound (MSUS) measures of the upper and lower extremity (UE and LE) joints. This study aimed to examine the association of BMI with clinical and MSUS joint assessments of the UE/LE joints in a large cohort of RA patients.
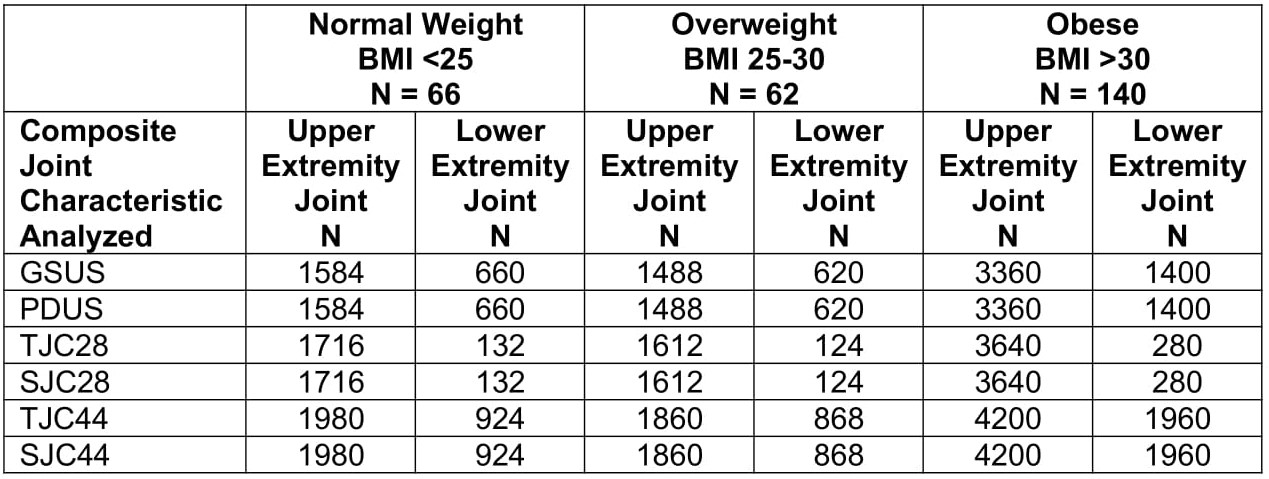
Methods: We examined a cross-sectional cohort of 268 patients meeting American College of Rheumatology 2010 RA classification criteria who completed screening visits for clinical trials. Patients were grouped by BMI: < 25, 25 to 30, and ≥ 30. Demographic data and DAS28/ESR were collected including 28 and 44 tender and swollen joint counts (TJC28, SJC28, TJC44, SJC44). Following the LAJAX protocol (Ben-Artzi et al. 2021), grayscale and power Doppler ultrasound (GSUS and PDUS) images were obtained from 34 joints: bilateral radioulnar joint midline of the wrists, proximal interphalangeal joints, interphalangeal joints, metacarpophalangeal joints, knees, and metatarsophalangeal joints (excluding MTP1). Each image was scored on a scale of 0-3. For joints with multiple views, the highest PDUS and GSUS score was used. Joints were categorized as either UE or LE. GSUS and PDUS scores were calculated by taking the average of all individual joint scores per UE or LE group. SJC and TJC scores were calculated using the proportion of swollen or tender joints out of all joints per UE or LE group. Differences between UE and LE joints for both ultrasound (GSUS and PDUS) and clinical joint measures (TJCs and SJCs) were calculated across BMI groups using t-tests. For each joint assessment, interaction effects were tested between UE/LE joint categories and BMI via analysis of variance (ANOVA).
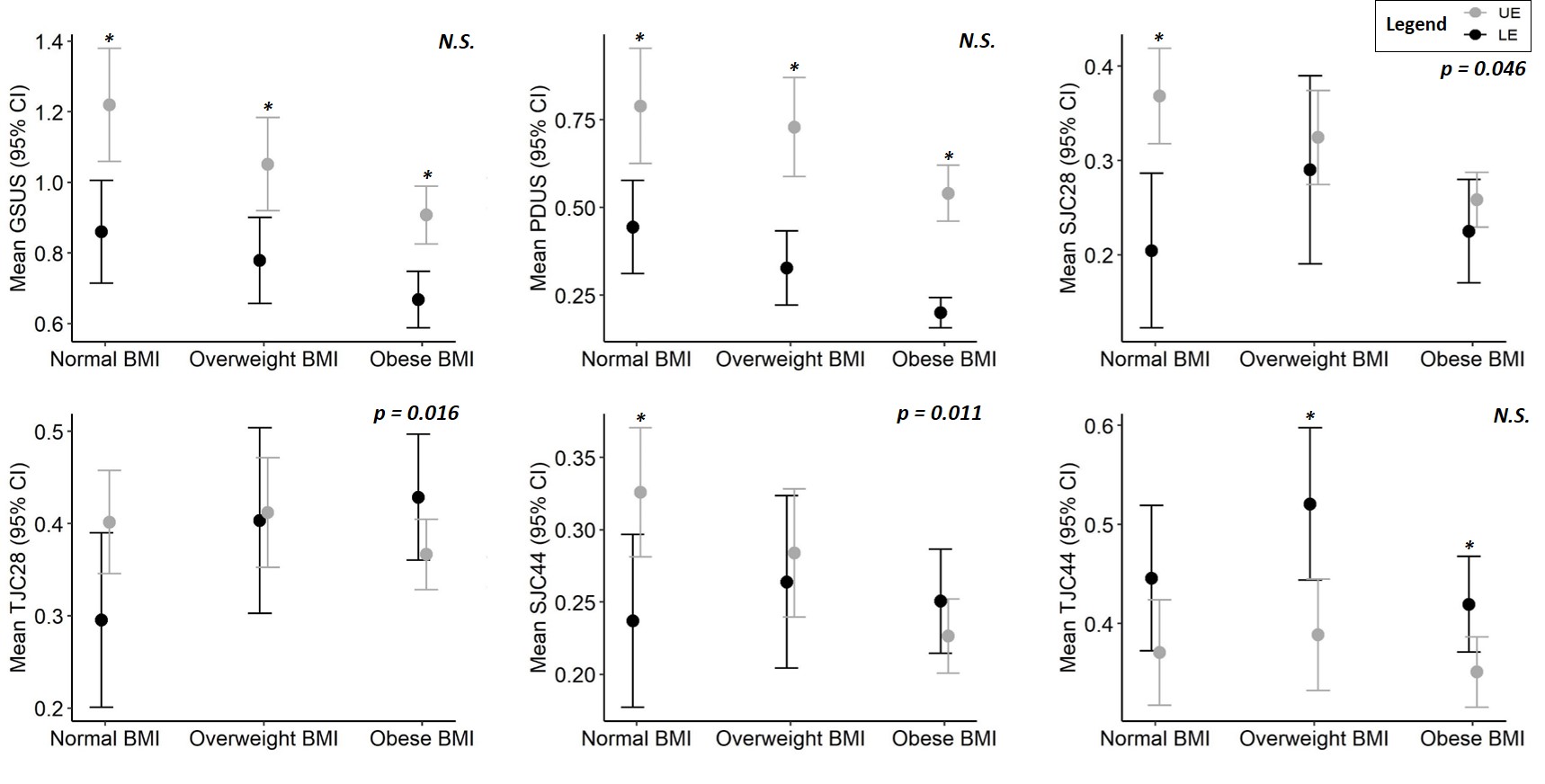
Results: Within the cohort, mean age was 54.8 years, 90.2% were female, 45% Caucasian, 78.7% seropositive and mean disease duration was 11.9 years. Patients overall had moderate disease activity with an average DAS28/ESR of 4.8. A total of 11,792 joints were examined by MSUS and/or joint counts. A breakdown of the UE and LE joint distribution per measure among BMI groups is shown in Table 1. Analyses comparing UE versus LE joints demonstrated a higher MSUS burden (GSUS and PDUS) in the UEs regardless of BMI (Figure 1) (p< 0.05), although there was not a significant UE/LE by BMI interaction (p>0.05). For SJC28 and SJC44 the UE/LE difference was significantly different across BMI categories (p< 0.05 for interaction). Normal weight patients had significantly higher joint swelling in the UEs (both p< 0.03), but this was not seen for overweight or obese patients (all p>0.05). Significant differences in individual joints of TJC28 for UE/LE were observed across BMI groups (p=0.02).
Conclusion: We observed a significant differential effect of BMI in the UE versus LE comparisons for clinical joint assessments (TJC 44, SJC 28, and SJC44), which are thought to be more subjective measures. However, for more objective measurements of joints by MSUS (PDUS and GSUS), this differential effect of UE/LE across BMI was not seen.
BMI = body mass index, N = number, GSUS = grayscale ultrasound, PDUS = power Doppler ultrasound, TJC28 = 28 tender joint count, SJC28 = 28 swollen joint count, TJC44 = 44 tender joint count, SJC44 = 44 swollen joint count.
N.S. = ANOVA not significant (p > 0.05), * = significant difference (p < 0.05), LE = lower extremity, UE = upper extremity, CI = confidence interval, BMI = body mass index, N = number, GSUS = grayscale ultrasound, PDUS = power Doppler ultrasound, TJC28 = 28 tender joint count, SJC28 = 28 swollen joint count, TJC44 = 44 tender joint count, SJC44 = 44 swollen joint count.
To cite this abstract in AMA style:
Morris N, Saab E, Chen L, Brook J, S Kaeley G, Elashoff D, Ranganath V. Impact of Body Mass Index (BMI) on Upper versus Lower Extremity Joints Assessed Using Clinical and Musculoskeletal Ultrasound Measures in Rheumatoid Arthritis Patients [abstract]. Arthritis Rheumatol. 2023; 75 (suppl 9). https://acrabstracts.org/abstract/impact-of-body-mass-index-bmi-on-upper-versus-lower-extremity-joints-assessed-using-clinical-and-musculoskeletal-ultrasound-measures-in-rheumatoid-arthritis-patients/. Accessed .« Back to ACR Convergence 2023
ACR Meeting Abstracts - https://acrabstracts.org/abstract/impact-of-body-mass-index-bmi-on-upper-versus-lower-extremity-joints-assessed-using-clinical-and-musculoskeletal-ultrasound-measures-in-rheumatoid-arthritis-patients/