Session Information
Date: Monday, November 13, 2023
Title: (1264–1307) RA – Diagnosis, Manifestations, and Outcomes Poster II
Session Type: Poster Session B
Session Time: 9:00AM-11:00AM
Background/Purpose: Rheumatoid arthritis (RA) patients with obesity are less likely to respond to therapy and achieve remission. Obesity is a known driver of inflammatory processes and is also associated with conditions such as osteoarthritis, fibromyalgia, and other comorbid conditions. The objective of this study was to comprehensively examine various disease activity measures (composite clinical measures, patient surveys, and musculoskeletal ultrasound (MSUS)) across BMI in a large RA cohort. Prior studies evaluating this question have been small with conflicting findings.
Methods: Clinical and MSUS data were obtained from 268 RA patients meeting American College of Rheumatology 2010 RA classification criteria who completed screening visits for RA clinical trials at an academic center. Patients were grouped by BMI categories: < 25, 25 to 30, and ≥ 30. Laboratory measurement of erythrocyte sedimentation rate (ESR), C-reactive protein (CRP), anti-cyclic citrullinated peptide (ACPA) and rheumatoid factor (RF) levels were performed. 28- and 44-joint count Disease Activity Scores using ESR (DAS28/ESR and DAS44/ESR), Health Assessment Questionnaire Disability Index (HAQ-DI) and Routine Assessment of Patient Index Data 3 (RAPID3) scores were calculated. Grayscale and power Doppler ultrasound (GSUS and PDUS) scores were calculated using the LAJAX 34 joint protocol (Ben-Artzi et al. 2021). Images were scored semi-quantitatively on a scale of 0–3. Total PDUS and GSUS scores were calculated via summation of all 34 joint scores (range 0–102). Demographic and clinical characteristics were categorized across BMI groups using the Kruskal-Wallis test (KW) for continuous variables and chi-square tests for categorical variables. Multiple linear regressions were used to assess factors influencing PDUS and GSUS.
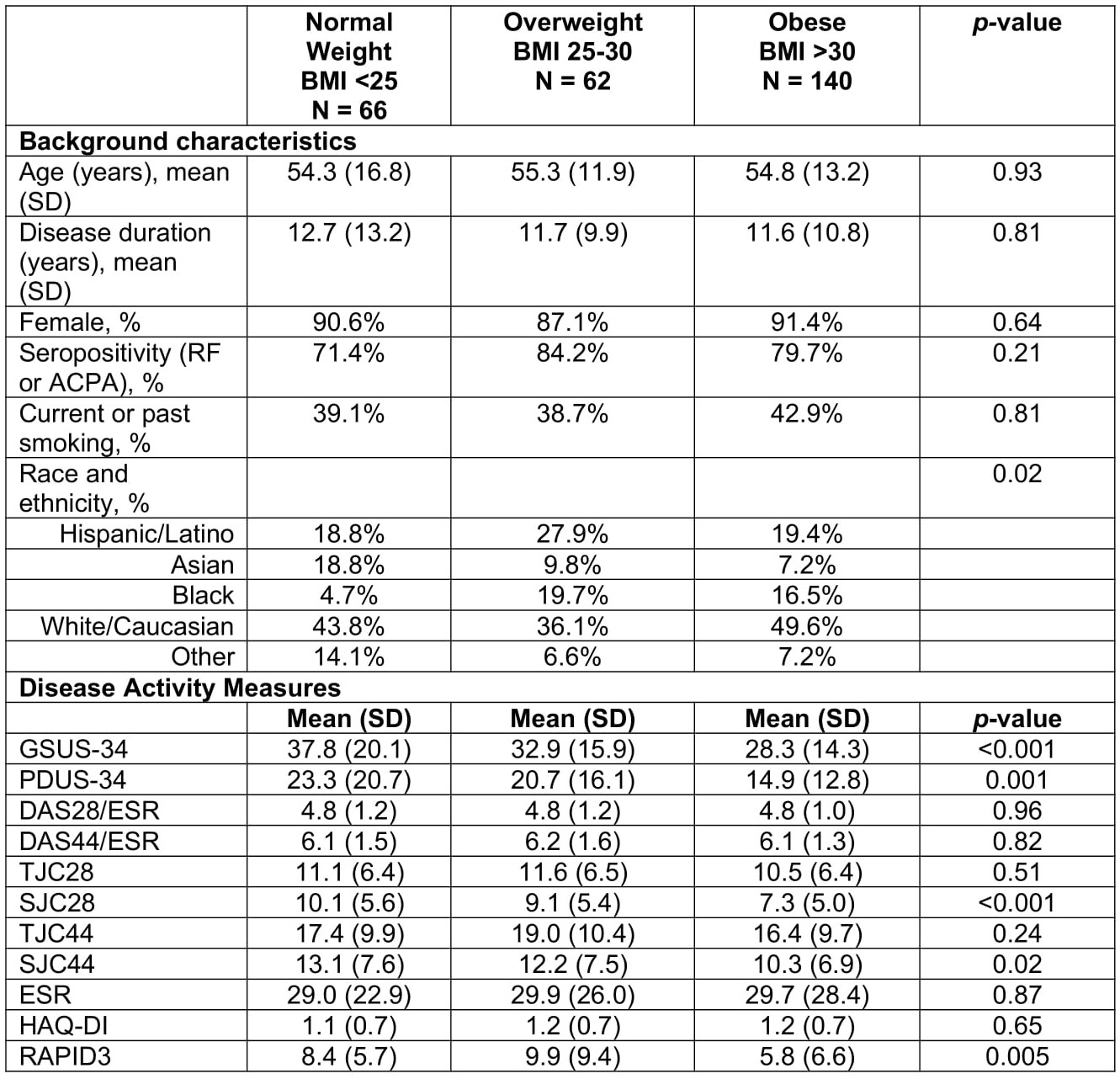
Results: Demographics were similar across BMI categories except for race/ethnicity (p=0.02). GSUS and PDUS scores significantly differed across BMI groups, with obese patients showing the lowest MSUS activity (p< 0.001 and p=0.001, respectively). DAS28/ESR, DAS44/ESR, TJC28, TJC44 were not different across BMI. However, SJC28 and SJC44 were significantly different across BMI groups and numerically lower in BMI >30. RAPID3 demonstrated a significant difference across BMI where obese patients were numerically lower, while HAQ-DI did not differ. In the regression models, BMI was significantly negatively associated with PDUS and GSUS after accounting for demographic characteristics, DAS28/ESR, disease duration, and seropositivity. In these models race, sex, smoking, seropositivity and DAS28/ESR were also significantly associated with MSUS findings.
Conclusion: In this large cohort of RA patients, DAS28/ESR and DAS44/ESR were similar across BMI categories. However, active synovitis as measured by PDUS and GSUS scores were independently negatively associated with BMI, after accounting for DAS and other demographic factors. These results suggest there is less MSUS joint inflammation in obese patients, which is consistent with prior findings of reduced radiographic damage observed in obese RA patients. Further study is warranted to confirm these findings.
BMI = body mass index, SD = standard deviation, RF = rheumatoid factor, ACPA = anti-cyclic citrullinated peptide, GSUS = grayscale ultrasound, PDUS = power Doppler ultrasound, TJC28 = 28 tender joint count, SJC28 = 28 swollen joint count, TJC44 = 44 tender joint count, SJC44 = 44 swollen joint count, DAS28/ESR = 28 joint disease activity score with erythrocyte sedimentation rate, DAS44/ESR = 44 joint disease activity score with erythrocyte sedimentation rate, HAQ-DI = Health Assessment Questionnaire Disability Index, and RAPID3 = Routine Assessment of Patient Index Data 3.
To cite this abstract in AMA style:
Morris N, Saab E, Chen L, Brook J, S Kaeley G, Elashoff D, Ranganath V. Impact of Body Mass Index (BMI) on Rheumatoid Arthritis Disease Activity and Musculoskeletal Ultrasound Measures [abstract]. Arthritis Rheumatol. 2023; 75 (suppl 9). https://acrabstracts.org/abstract/impact-of-body-mass-index-bmi-on-rheumatoid-arthritis-disease-activity-and-musculoskeletal-ultrasound-measures/. Accessed .« Back to ACR Convergence 2023
ACR Meeting Abstracts - https://acrabstracts.org/abstract/impact-of-body-mass-index-bmi-on-rheumatoid-arthritis-disease-activity-and-musculoskeletal-ultrasound-measures/