Session Information
Session Type: Poster Session D
Session Time: 1:00PM-3:00PM
Background/Purpose: Interstitial lung disease (ILD) in primary Sjögren’s syndrome (pSS) has been reported to be present in 10-15% of patients, but ILD progression in pSS-ILD has not been assessed in detail. The objective of this study was to assess ILD progression in pSS and factors associated with disease progression in a well-characterized pSS-ILD cohort.
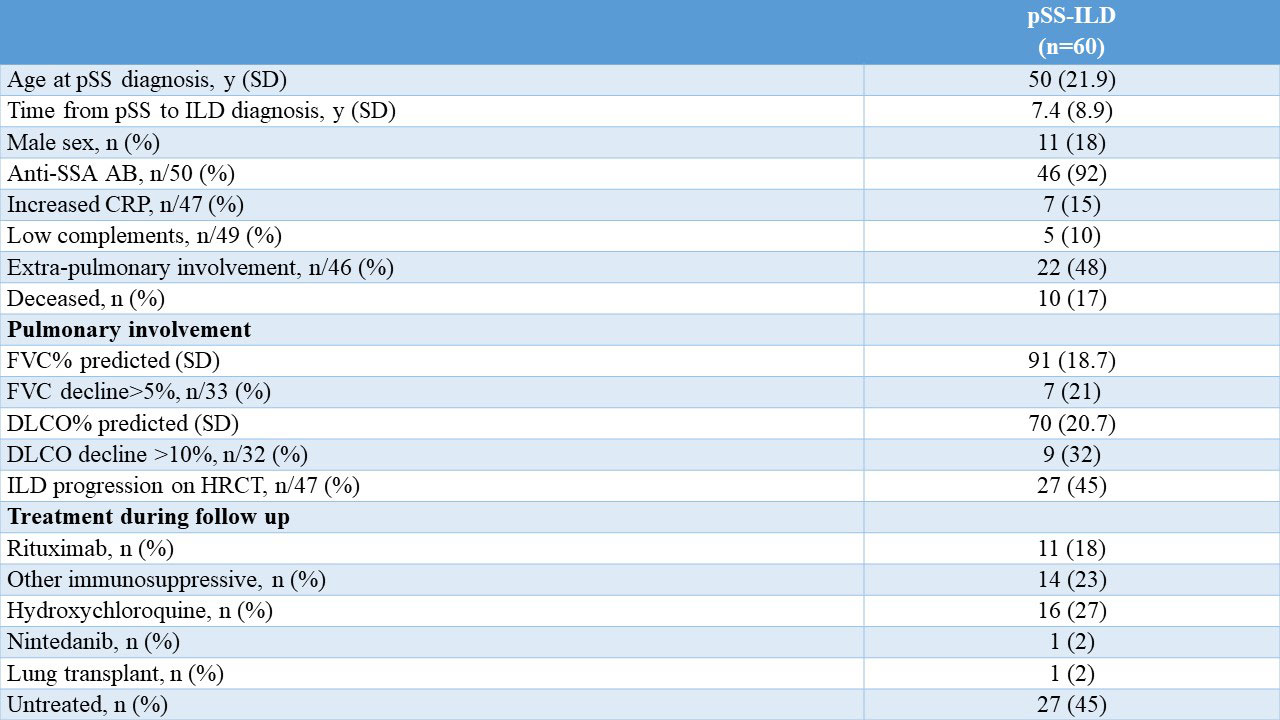
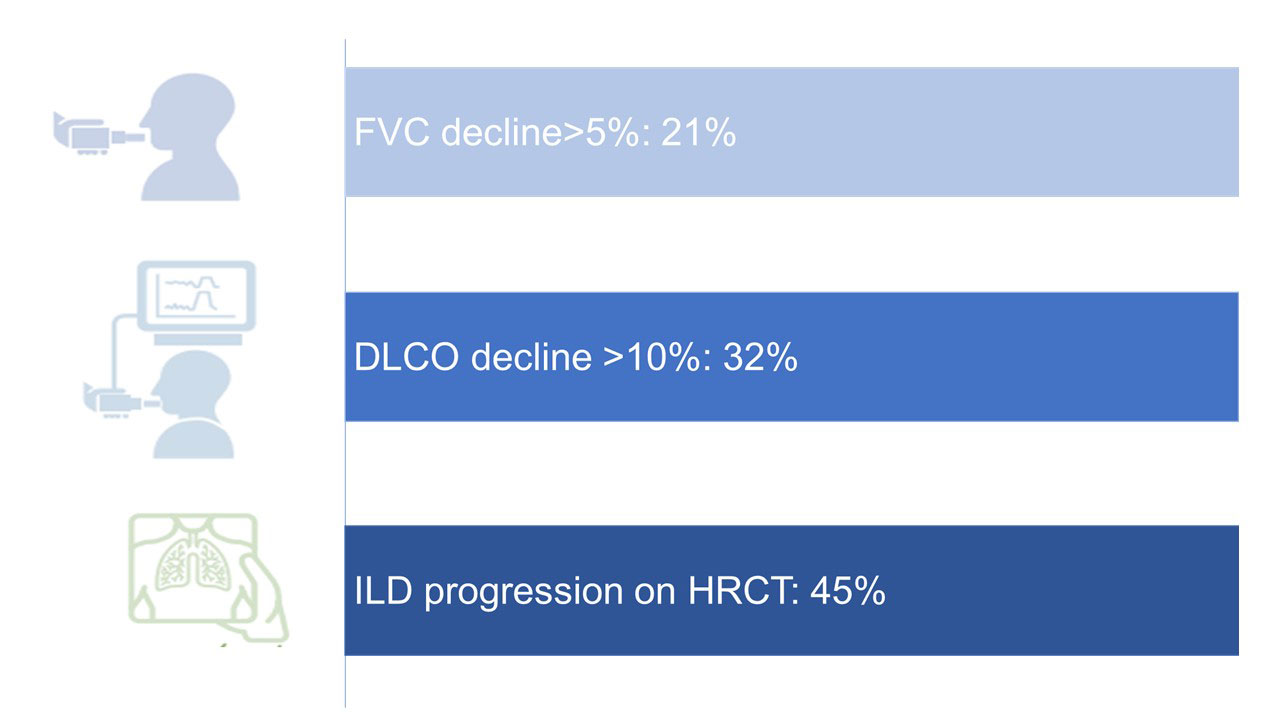
Methods: All pSS patients with ILD diagnosed on HRCT from the Oslo University Hospital (OUH) were included. Clinical characteristics, treatment (including rituximab, other immunosuppressives, hydroxychloroquine, nintedanib and lung transplantation), lung function tests including forced vital capacity (FVC) and diffusing capacity for carbon monoxide (DLCO), and ILD pattern on HRCT assessed by a radiologist were evaluated. We determined ILD progression defined as (1) absolute FVC decline >5%; or (2) absolute DLCO decline >10% over 12 +/-6 months; or (3) increasing extent of ILD on HRCT over the observation period. Potential risk factors associated with disease progression were chosen based on expert opinion. Descriptive analyses were conducted.
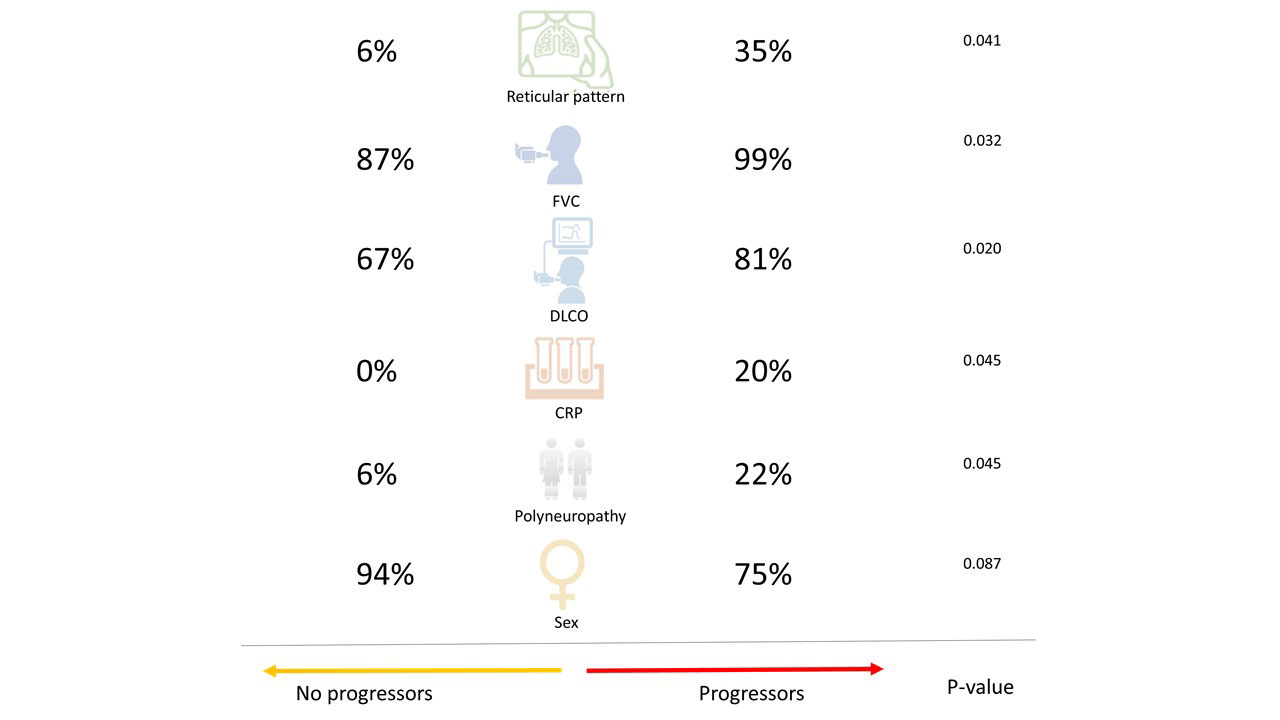
Results: Of 702 pSS patients followed at OUH, we identified 60 pSS patients with ILD with 33 (55%) having followup at 12 months (Table). Mean time from pSS to ILD diagnosis was 7.4 years. In 67% ILD was diagnosed after pSS, in 13% simultaneously, and in 11% before pSS diagnosis. In total, 28 (47%) had lymphocytic interstitial pneumonia (LIP) and 32 (53%) reticular pattern on HRCT. Of all, 33 (53%) were treated (Table). Over mean followup of 10.9 months (SD 4.2), 7/33 (21%) showed FVC >5% decline, 9/32 (28%) DLCO >10% decline and 12 (36%) had at least one of these defined lung function declines on standard of care treatment (Figure 1). Over an observation period of 15.4 (SD 10.6) years, 27/47 (45%) showed any ILD progression on HRCT (Figure 1). HRCT pattern was not associated with risk of >10% DLCO decline or ILD progression on HCRT. >5% FVC decline occurred more frequently in patients with reticular pattern compared to LIP (6/17 (35%) vs 1/16 (6%), p=0.041). Factors significantly associated with ILD progression on lung function (either FVC eller DLCO decline) included higher baseline FVC (99% (SD16.4) vs 87% (SD14.9), p=0.032), higher DLCO (81% (SD13.1) vs 67% (SD17.4), p=0.020), increased CRP (2/10 (20%) vs 0/16 (0%), p=0.045), presence of polyneuropathy (2/9 (22%) vs 1/17 (6%), p=0.045) and numerically male sex (2/12 (25%) vs 1/21 (6%), p=0.087) (Figure 2). Treatment was not associated with ILD progression.
Conclusion: A substantial number of patients with pSS-ILD progressed on standard of care treatment. This highlights the importance of close monitoring and active consideration of treatment initiation and escalation in pSS-ILD.
To cite this abstract in AMA style:
Hoffmann-Vold A, Fretheim H, Diep P, Lerang K, Gudbransson B, Andersson H, Midtvedt Ø, Garen T, Durheim M, Aaløkken T, Palm Ø, Molberg Ø. ILD Associated with Primary Sjögren’s Syndrome Is Frequently Progressive [abstract]. Arthritis Rheumatol. 2022; 74 (suppl 9). https://acrabstracts.org/abstract/ild-associated-with-primary-sjogrens-syndrome-is-frequently-progressive/. Accessed .« Back to ACR Convergence 2022
ACR Meeting Abstracts - https://acrabstracts.org/abstract/ild-associated-with-primary-sjogrens-syndrome-is-frequently-progressive/