Session Information
Session Type: Poster Session A
Session Time: 10:30AM-12:30PM
Background/Purpose: Vision loss occurs in 50% of children with chronic anterior uveitis (CAU). Lack of symptoms and overt ocular signs of inflammation may lead to delayed diagnosis and contribute to poor visual outcomes. Anterior segment inflammation is detected and quantified by slit lamp examination using the Standardization of Uveitis Nomenclature (SUN). Accurate assessment is subjective and may be especially difficult in children who are uncooperative with the exam. Frequent serial exams may also be burdensome to patients and families. Biomarkers that reflect ocular inflammation in aqueous humor have been detected in the tear fluid. Tear fluid collection is a noninvasive method to detect biomarkers that reflect intraocular inflammation and may improve medical decision-making and prognosis of children with CAU. We aim to identify biomarkers in tear fluid of children with CAU that reflect changes in CAU activity.
Methods: For our prospective study, we collected tear samples by Schirmer strips from children with CAU at two time points – active (AC cell ≥ 0.5+) and inactive (AC cell =0) as defined by the SUN criteria. Proteins were measured in tear fluid by tandem mass tag (TMT) labeling and nanoLC-MS/MS and normalized by total peptide amount. A logarithmic transformed average of 2 abundance readings per protein/subject was used. We compared proteins in children during active and inactive CAU using a Wilcoxon rank sum test (p-value< 0.1), and then stratified the analysis based on the underlying disease (JIA-associated uveitis [JIA-U]) and idiopathic CAU [iCAU]).
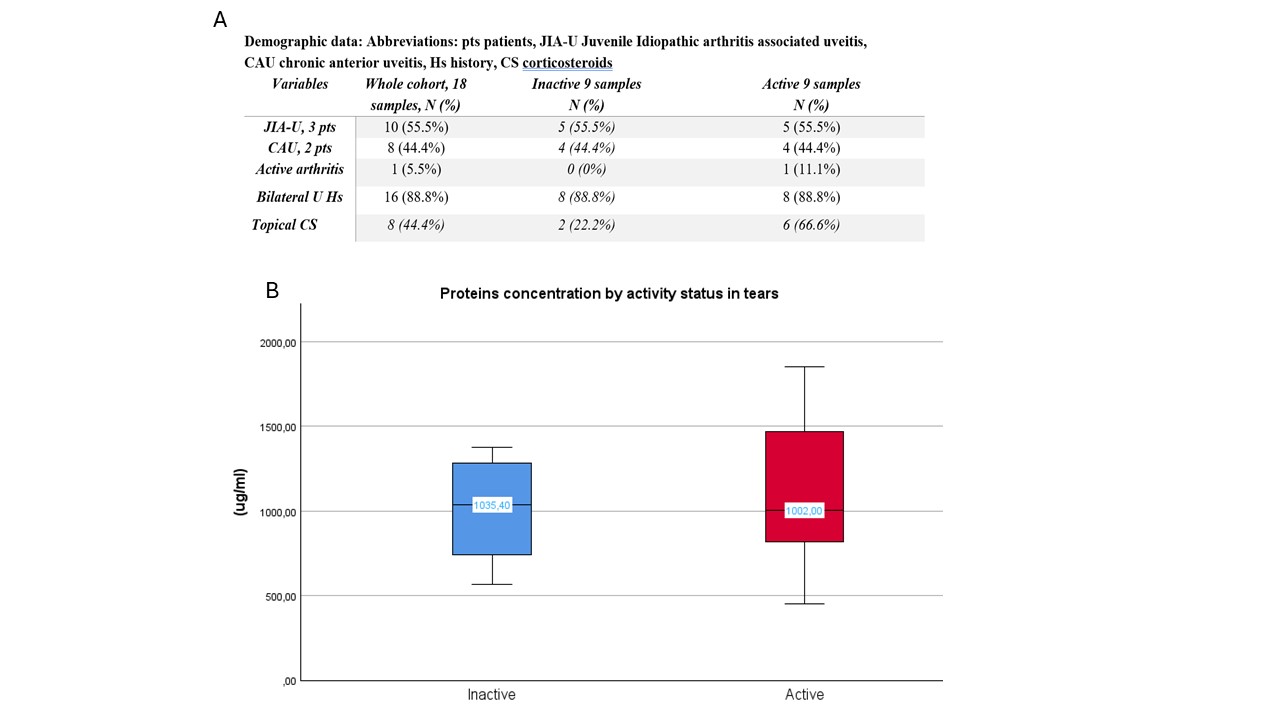
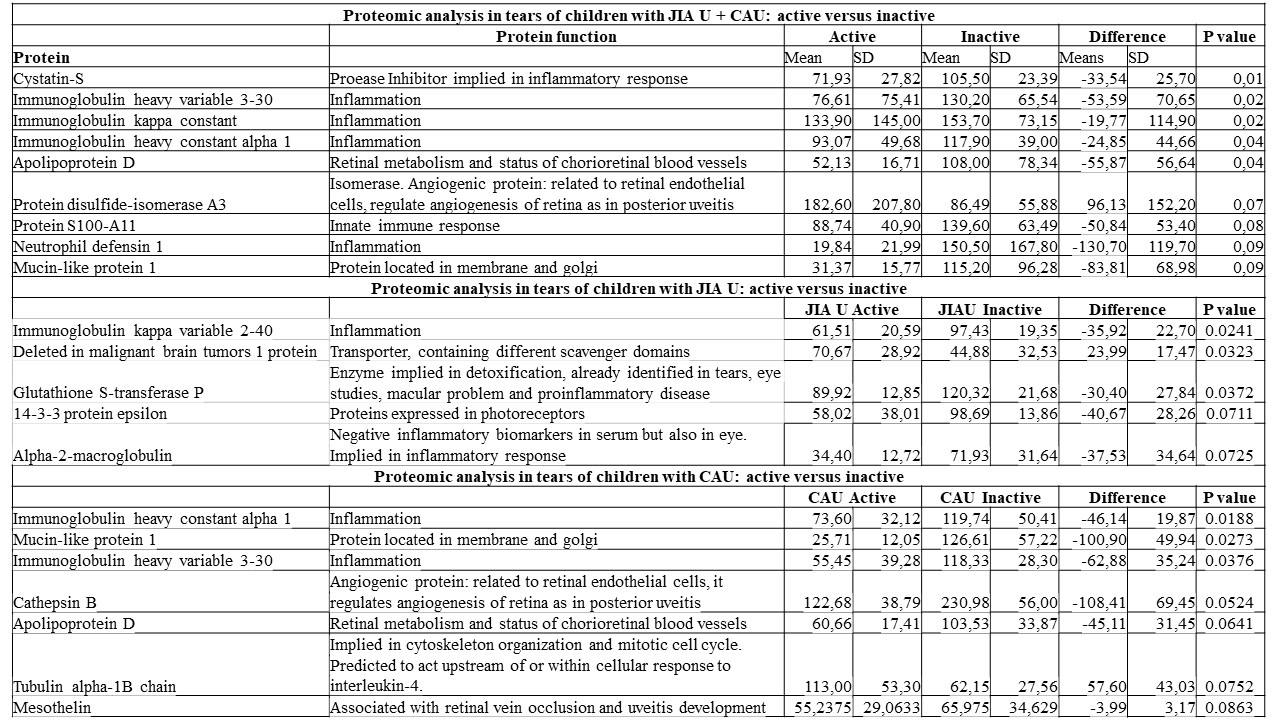
Results: Eighteen paired tear samples were collected (9 active and 9 inactive) from 3 JIA-U children (10 samples) and 2 iCAU (8 samples) (Figure 1A). Eight eyes (44.4%) required topical corticosteroids. 241 proteins were identified at medium 95% or higher FDR confidence with at least 1 high confidence peptide. The number of proteins detected was similar in children with active and inactive CAU (median 1035 vs 1002, p 0.75, Figure 1), even after stratifying by CAU diagnosis (JIA-U median 1035 vs 1002, P value=0.75; iCAU median 1114 vs 1212, P value=1). When we compared all children with CAU, we identified 9 proteins distinguishing children with active from inactive CAU irrespective of CAU type (Table 1). After stratifying the analysis by CAU diagnosis, we identified other candidate protein biomarkers (Table: 5 for JIA-U and 7 for CAU). Several of these have been associated with uveitis, are pro-inflammatory, and are related to the immune system (Table 1).
Conclusion: Several candidate biomarkers of ocular inflammation reflect changes in CAU activity as seen on slit lamp examination within patients over time. Given the challenges of clinical examination, biomarkers that reflect the course of CAU could augment ocular surveillance and inform the adequacy of treatment. CAU is vision-threatening and warrants exploration of techniques for accurate monitoring of inflammation to promptly inform immunosuppressive treatment. Objective and reliable measures to assess inflammation may aid in the management of these patients and improve visual outcomes.
To cite this abstract in AMA style:
Maccora I, brunner h, Altaye M, Duell A, Haffey W, Quinlan-Waters M, Sproles A, Thornton S, Miraldi Utz V, Greis K, Angeles-Han s. Identification of Protein Biomarkers in Tear Fluid of Children with Uveitis That Distinguishes the Ocular Inflammatory State [abstract]. Arthritis Rheumatol. 2024; 76 (suppl 9). https://acrabstracts.org/abstract/identification-of-protein-biomarkers-in-tear-fluid-of-children-with-uveitis-that-distinguishes-the-ocular-inflammatory-state/. Accessed .« Back to ACR Convergence 2024
ACR Meeting Abstracts - https://acrabstracts.org/abstract/identification-of-protein-biomarkers-in-tear-fluid-of-children-with-uveitis-that-distinguishes-the-ocular-inflammatory-state/