Session Information
Session Type: Poster Session C
Session Time: 9:00AM-11:00AM
Background/Purpose: Elevated serum uric acid (SUA) level is rather prevalent in the general population, and it is associated with numerous comorbidities and mortality. Etiology of hyperuricemia seems to play a role in hyperuricemia-associated morbidity and mortality risk. Metabolic hyperuricemia (elevated SUA mainly due to urate overproduction) is found to be more dangerous than renal hyperuricemia (elevated SUA due to renal underexcretion of uric acid).1 There has however been only few studies done on the association between hyperuricemia and fatty liver and it is not known if the different types of hyperuricemia affect the fatty liver risk differently.
Methods: We used data from GOAL (Good Ageing in Lahti region) study – a prospective, population-based study of elderly Northern European individuals (52–76 years). Data of SUA levels and other laboratory parameters, comorbidities, lifestyle habits and socioeconomic factors were collected. Persons with SUA values of >410 μmol/L (≈6.9 mg/dL; 75th percentile) are represented as clearly hyperuricemic. In those that are clearly hyperuricemia, we defined hyperuricaemia renal if estimated glomerular filtration rate (eGFR) was ≤67 ml/min (25th percentile) and metabolic if eGFR was >67 ml/min. Glomerulal filtration rate was calculated using CKD-EPI creatinine-cystatin C equation. Fatty liver index (FLI) is an accurate predictor of hepatic steatosis and it was calculated from body mass index, waist circumference, triglyceride, and gamma-glutamyl transferase data.2 Persons with FLI ≥80 (75th percentile) are represented as having a very high probability of fatty liver. The results for mortality in the 15-year follow-up period were adjusted for age, sex, education, smoking status, alcohol consumption, body mass index, hypertension, dyslipidemia, and diabetes.
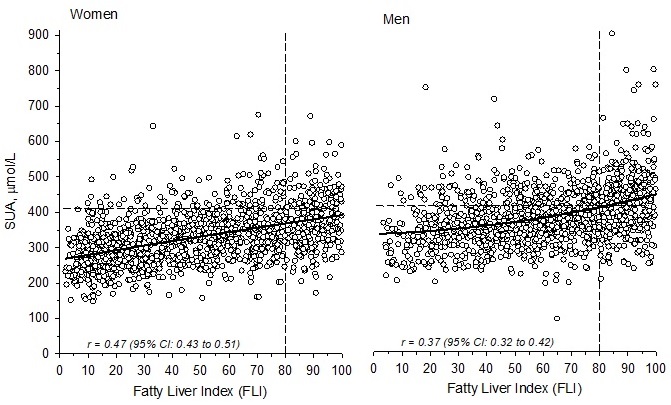
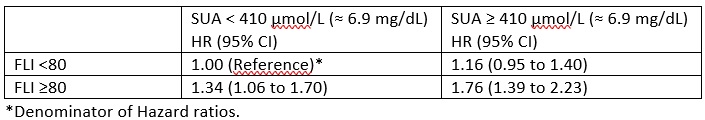
Results: There is a clear correlation between FLI and SUA in both women [r=0.47 (95% CI =0.43-0.51)]and men [r=0.37 (95% CI =0.32-0.42)], see figure 1. Mortality was higher in individuals with FLI ≥80 than in those with FLI < 80 both in clearly hyperuricemic and slightly hyperuricemic/normouricemic persons. When compared to individuals with SUA ≤410 μmol/L (≈6.9 mg/dL) and FLI < 80 the hazard ratio (HR) for all-cause mortality was 1.76 (95% CI: 1.39 to 2.23) in clearly hyperuricemic persons with FLI ≥80, 1.16 (95% CI: 0.95 to 1.40) in clearly hyperuricemic persons with FLI < 80 and 1.34 (95% CI: 1.06 to 1.70) in persons with SUA ≤ 410 μmol/L (≈6.9 mg/dL) and FLI ≥80 (table 1). Individuals with metabolic hyperuricemia had a statistically significantly higher FLI than individuals with renal hyperuricemia: mean (SD)=73.4 (12.2) and 69.6 (22.5), respectively, p=0.015 after adjusting for sex and diabetes.
Conclusion: Fatty liver positively correlates with serum uric acid level. Both fatty liver and hyperuricaemia increase mortality and the most dangerous is a combination of both conditions. Regarding development of fatty liver “metabolic hyperuricemia” appears to be more hazardous than “renalhyperuricemia” since it associates with higher FLI.
1Timsans J, et al. Annals of the Rheumatic Diseases 2023;82:2067-2068.
2Bedogni G, et al. BMC Gastroenterol. 2006;6:33.
To cite this abstract in AMA style:
Timsans J, Kauppi J, Kautiainen H, Kauppi M. Hyperuricemia – Especially “Metabolic Hyperuricemia” – Is Independently Associated with Higher Risk of Fatty Liver [abstract]. Arthritis Rheumatol. 2023; 75 (suppl 9). https://acrabstracts.org/abstract/hyperuricemia-especially-metabolic-hyperuricemia-is-independently-associated-with-higher-risk-of-fatty-liver/. Accessed .« Back to ACR Convergence 2023
ACR Meeting Abstracts - https://acrabstracts.org/abstract/hyperuricemia-especially-metabolic-hyperuricemia-is-independently-associated-with-higher-risk-of-fatty-liver/