Session Information
Session Type: Poster Session B
Session Time: 8:30AM-10:30AM
Background/Purpose: Physicians share responsibilities to promote social justice and assure equitable healthcare for all. Street medicine (SM) is a field dedicated to address the need of homeless patients, often by visiting them in the street or anywhere they reside to deliver care. We, rheumatologists and SM providers, have been interested in identifying and improving the management and outcomes of our homeless RA patients. They do not fit available treatment guidelines or recommendations. Nor do many patients worldwide who, for challenges including distance, transportation, disabilities, income, and insurance, have limited access to care and medications. Therefore, with the encouragement of the SM Institute, we propose guidelines for rheumatologists and non-rheumatologists seeing these patients.
Methods: We adapted procedures for guidelines development from the ACR. A leadership team, of senior rheumatology faculty with extensive experience, including with guidelines, in RA (RSP) and SM (CF, BF), examined the available evidence. A research team critically reviewed the pertinent literature, synthesized the discussion, and formulated guiding principles and PICO (population, intervention, comparator, and outcome) for possible regimens (NZW, AA, BR, SH). For each PICO question, the panel reviewed evidence and provided recommendations. Also assessed were data about therapies’ efficacy, potential toxicities, ease of administration and monitoring, cost, and likely availability. The authors communicated through a series of questions focused on describing their approaches to affected patients.
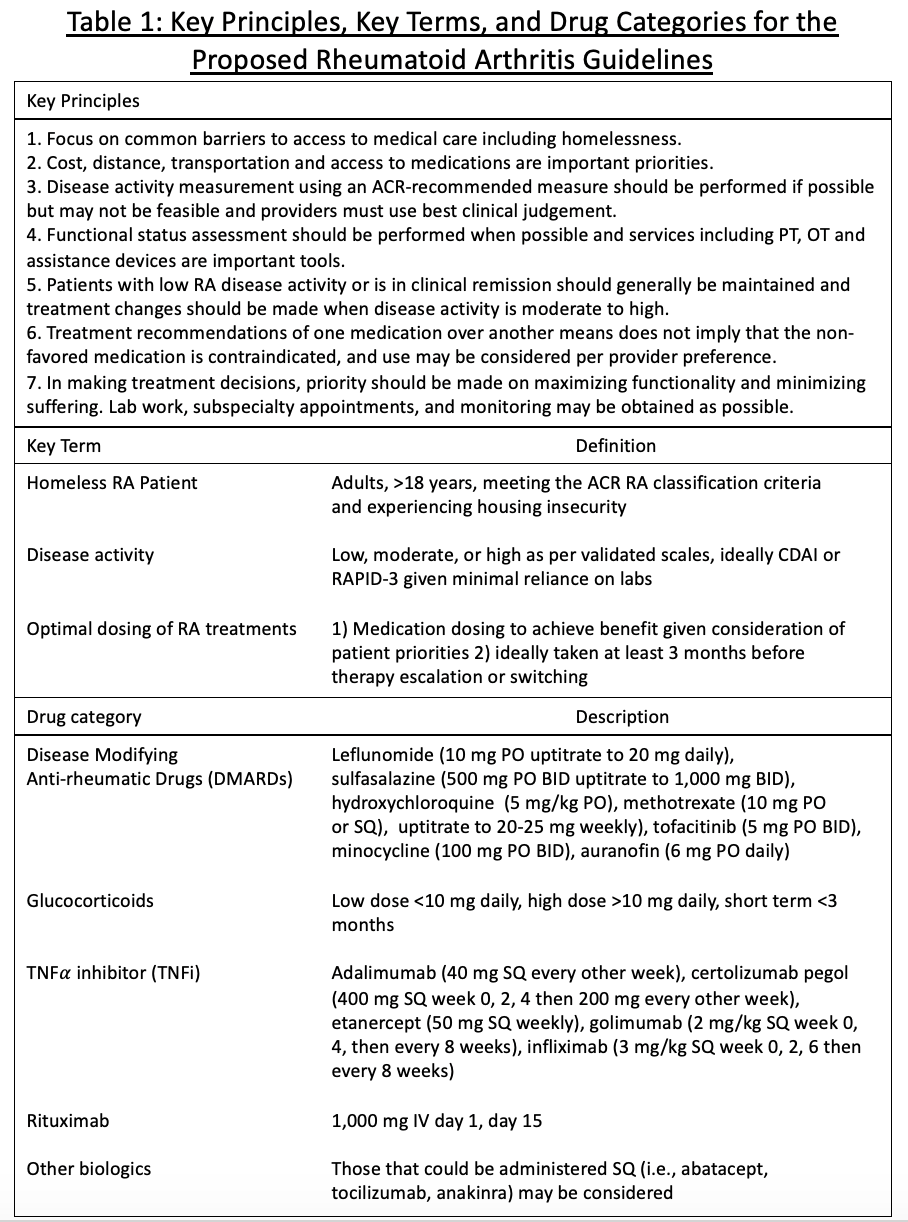
Results: The Table summarizes key principles, terms, descriptions, and drug categories. We developed the principles outlined in Figure 1, which are based on patients’ inability to consistently access rheumatologists; obtain, take, and store medications reliably; or get routine laboratory (or other) studies. Initial treatment regimens include leflunomide and sulfasalazine; alternatives are hydroxychloroquine, minocycline, methotrexate, auranofin, steroids (intermittently, low dose, or IA/IM), janus kinase inhibitors, and, for some, rituximab or other biologics. Figure 2 presents a proposed algorithm for continuity of care, individualized to patients’ contexts. Referrals for certain adjunctive/assistance equipment are included.
Conclusion: Our efforts to care for our homeless patients led us to consider what is minimally adequate or acceptable rheumatologic care, how is it defined and quantified, and how might we conceive more innovative ways to provide/deliver it or its equivalent (i.e., SM, tele-medicine, or other). We propose guidelines for providers caring for those vulnerable patients unable to see rheumatologists or follow current treatment regimens, those for whom available guidelines do not apply or are not realistic. SM practice and limited experience with homeless patients suggest that our proposed approach could be salutary for those patients worldwide who are challenged to see a rheumatologist or use (some of) our medications.
To cite this abstract in AMA style:
Zagelbaum Ward N, Amarnani A, Rai B, Feldman C, Feldman B, Panush R. How Might We Care for Rheumatoid Arthritis (RA) Patients Unable to See a Rheumatologist And/or Use Certain of Our Medications? Proposed Preliminary Recommendations for RA Patients Who Don’t Meet Our Established Guidelines [abstract]. Arthritis Rheumatol. 2021; 73 (suppl 9). https://acrabstracts.org/abstract/how-might-we-care-for-rheumatoid-arthritis-ra-patients-unable-to-see-a-rheumatologist-and-or-use-certain-of-our-medications-proposed-preliminary-recommendations-for-ra-patients-who-dont-me/. Accessed .« Back to ACR Convergence 2021
ACR Meeting Abstracts - https://acrabstracts.org/abstract/how-might-we-care-for-rheumatoid-arthritis-ra-patients-unable-to-see-a-rheumatologist-and-or-use-certain-of-our-medications-proposed-preliminary-recommendations-for-ra-patients-who-dont-me/