Session Information
Session Type: Abstract Session
Session Time: 10:00AM-10:50AM
Background/Purpose: The natural history of reactive arthritis (ReA) remains poorly understood. Certain patients with ReA will go on to develop a chronic course while others will have a self-limited course. The goal of this study is to identify prognostic factors for chronicity of disease.
Methods: ReA patients were identified via two methods; from a Spondyloarthritis clinic database and from an urgent Rheumatology clinic, both located within the University Health Network in Toronto, Canada. Baseline data at presentation, including history, physical exam, X-rays and clinical laboratory results were collected. Patients whose arthritis resolved and were discharged from clinic were defined as self-limited ReA, whereas patients with persisting arthritis with long term follow-up in the clinic were defined as chronic ReA.
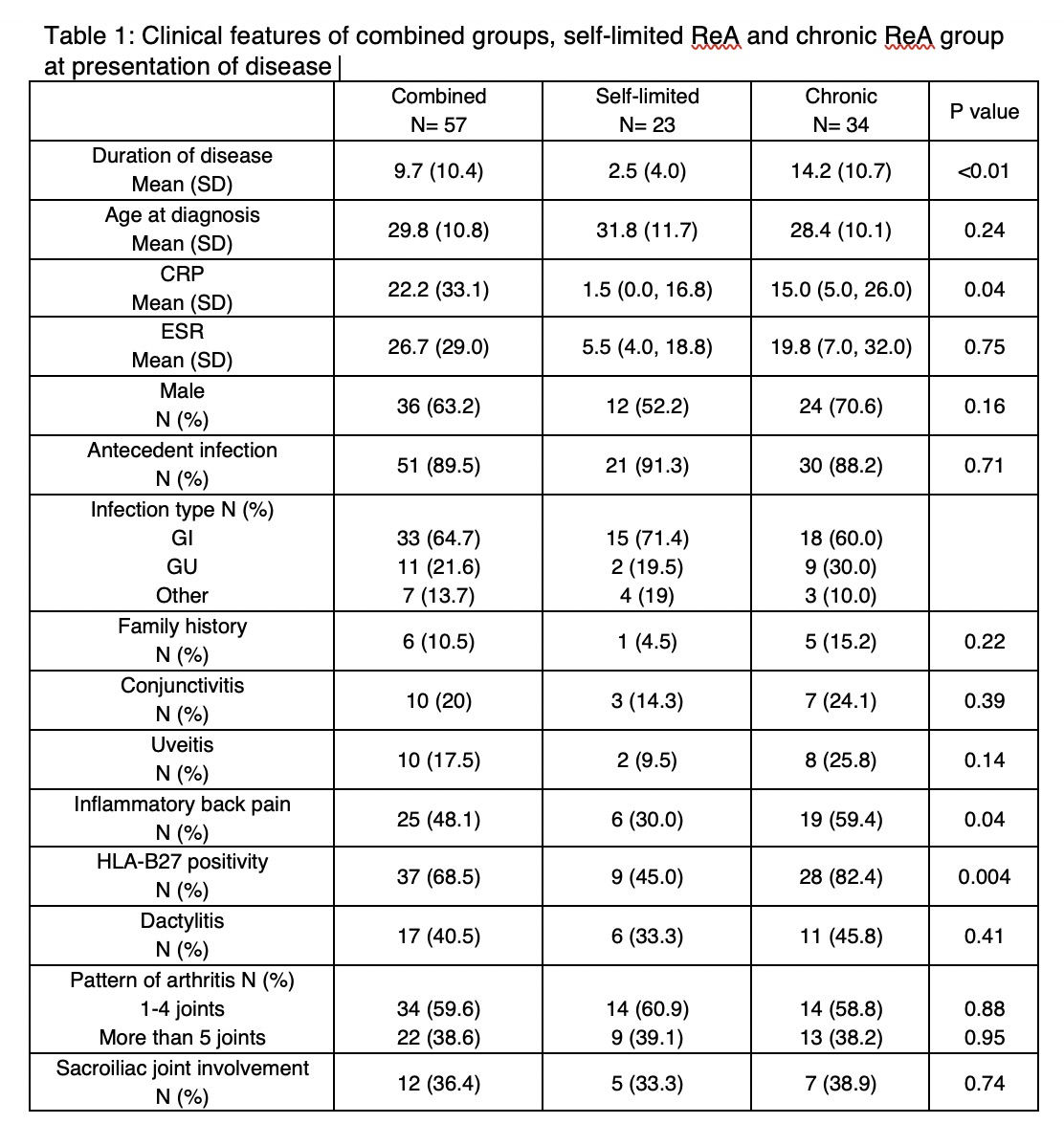
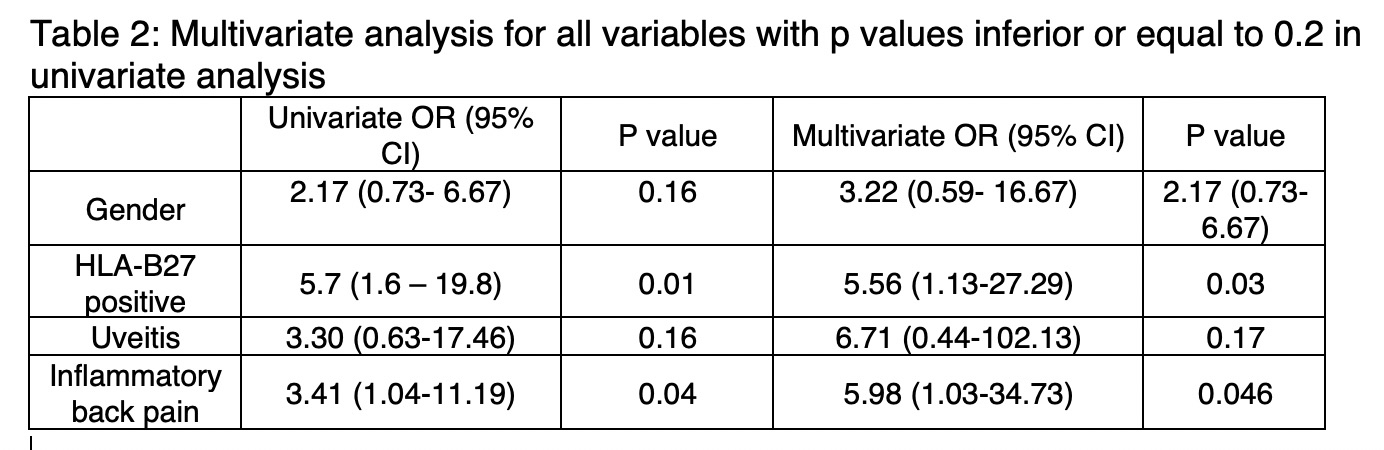
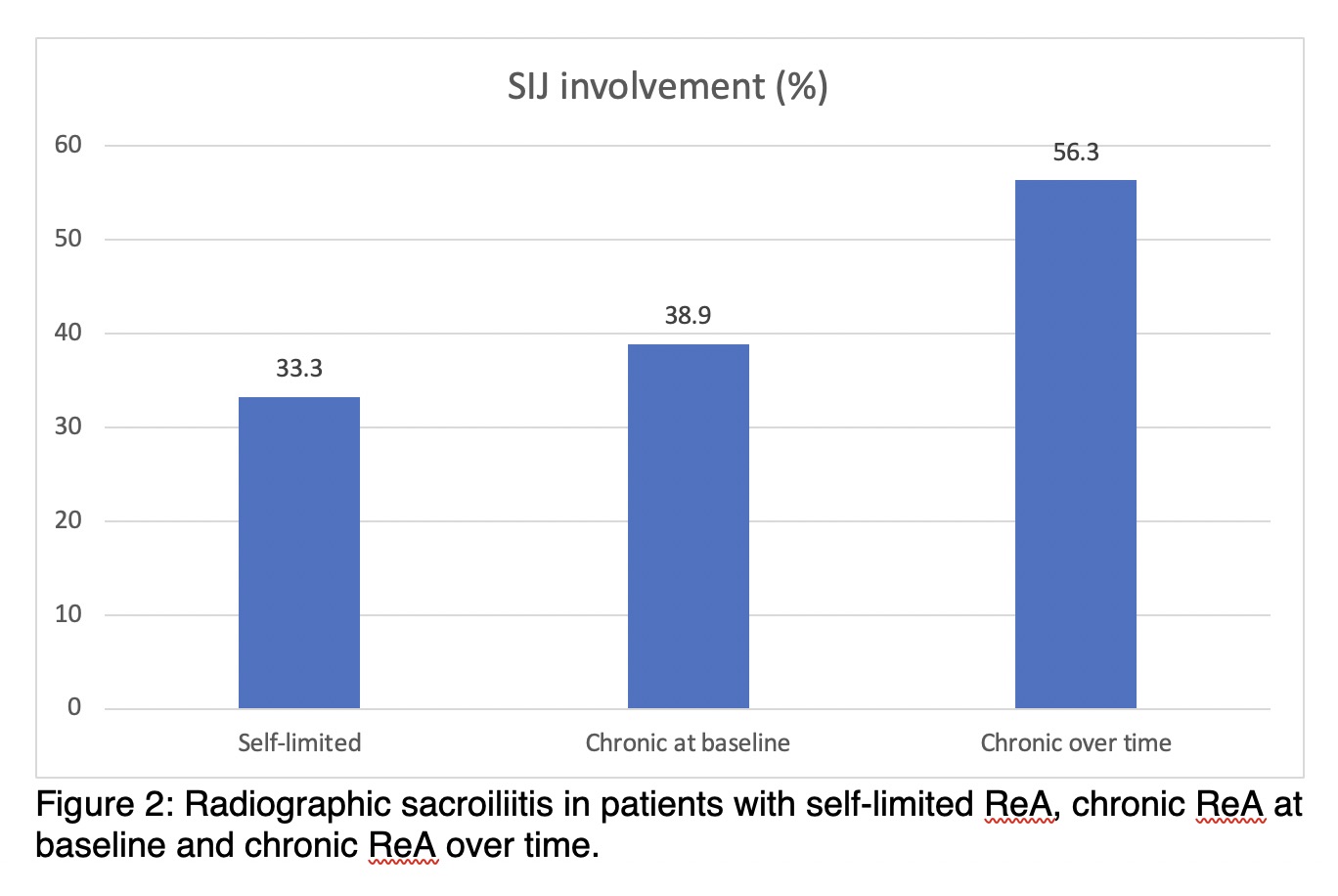
Results: A total of 57 patients with ReA were identified. Of these patients, 23 were classified as self-limited ReA (mean disease duration 2.5 years +/- 4.0) and 34 were classified as chronic ReA (disease duration 14.2 years +/- 10.7), p < 0.01. The most striking difference was the presence of HLA-B27: 82.4% in the chronic group vs45.0% in the self-limited (p= 0.004). The nature of the antecedent infection was not a prognostic marker. There was a difference in the presence of inflammatory back pain at disease onset (59.4% vs 30.0% p= 0.04) and in CRP (15.0 mg/L vs 1.5, p = 0.04) in the chronic vs self-limited group, respectively. In multivariate analysis, the presence uveitis trended towards an increased risk of chronic ReA (OR 6.71 (95% CI 0.44-102.12) as did male gender (OR 3.22 (95% CI 0.59- 16.67), but neither reached statistical significance. A subgroup analysis of chronic ReA patients revealed an increased incidence of both uveitis and SI joint involvement over time; 25.8% patients presented with uveitis; however over time, 53.9% developed uveitis. Similarly, 38.9% of chronic ReA patients initially presented with sacroiliitis vs. 56.3% over time.
Conclusion: HLA-B27 is the predominant risk factor for chronicity in ReA, as it is for ankylosing spondylitis (AS). In contrast, the type of antecedent infection is not a prognostic factor for the course of ReA. This suggests that host immune response orchestrated by HLA-B27, rather than a particular antigenic specificity, determines outcome in ReA by setting stage for chronic inflammation. This may have direct relevance to deciphering the inciting events in AS.
To cite this abstract in AMA style:
Wojcik S, Morris D, Fitzgerald G, Ramkissoon S, Haroon N, Inman R. HLA-B27 and Host Immune Response: Lessons from Reactive Arthritis [abstract]. Arthritis Rheumatol. 2020; 72 (suppl 10). https://acrabstracts.org/abstract/hla-b27-and-host-immune-response-lessons-from-reactive-arthritis/. Accessed .« Back to ACR Convergence 2020
ACR Meeting Abstracts - https://acrabstracts.org/abstract/hla-b27-and-host-immune-response-lessons-from-reactive-arthritis/