Session Information
Date: Friday, November 6, 2020
Session Type: Poster Session A
Session Time: 9:00AM-11:00AM
Background/Purpose: To validate high-sensitivity PET/CT as a diagnostic test we have explored the association of total-body and extremity PET/CT measures with the standardized psoriatic arthritis (PsA) outcome measures (DAPSA, Leeds Enthesitis Index, etc). The objective of our study is to determine the association of in vivo PET/CT measures, and use these data to create a catalog of systemic PsA musculoskeletal pathologies and compare with that of RA and OA.
Methods: Patients with RA, PsA or OA were enrolled in IRB-approved studies. All subjects underwent a single-timepoint PET/CT scan on either the total body uEXPLORER scanner or the UC Davis extremity PET/CT scanner for 20 minutes starting at either 40 or 70 minutes after IV injection of 18F-FDG (~1/4th of the conventional dose). Qualitative findings and different patterns for the three conditions were evaluated. We quantified the degree of inflammation in the extremities and whole-body, respectively and determine pathologic predilection for anatomical domains of bones/ligaments of hands in PsA, RA and OA.
Results: Here we will share data from recruited 20 patients, all males, with RA (n=7; median age: 67 years), PsA (n=10; median age: 68 years), OA (n=3; median age: 60 years). The RA patients had symmetric joint involvement, most commonly in the hands/knees. The following sites were involved: radio-and/or ulno-carpal compartments (n=5), MCP (n=4), PIP (n=5) joints. Joints of the feet appeared to be less frequently affected. All PsA patients demonstrated multiple sites of enthesitis (n=10/10), affected the tendons of the hands/fingers and seemed more active on the extensor side (n=5). Increased nail matrix/fingernail FDG uptake was observed to be a distinct feature (n=8/10). Several large joints showed positive findings in all patients. Less frequent features included sausage finger (n=2), plantar fasciitis (n=3); sacroiliac joint (n=2). Involvement of the interspinous ligament (n=2) and facet joints (n=2) was also noted. Patients with OA showed unilateral enhanced FDG uptake at least one big joint (shoulder, n=3; elbow, n=1; knee, n=2), and small joints of the hand/feet (1st CMC/1st MTP).
Conclusion:
- Asymmetric synovitis of small joints of hands/feet, enthesitis, nail matrix inflammation, dactylitis and spondylitis stands out to be pathologic features for PsA.
- There appeared to be an overall concurrence between degree of inflammation by imaging and clinical outcome measures of PsA such as DAPSA and Leeds Enthesitis Index.
- We expect at the completion of this study these clinico-radiologic domains will provide for unique quantitative diagnostic imaging biomarkers for PsA and a single PET imaging scan will be able to differentiate from other inflammatory/non-inflammatory conditions like RA and OA.
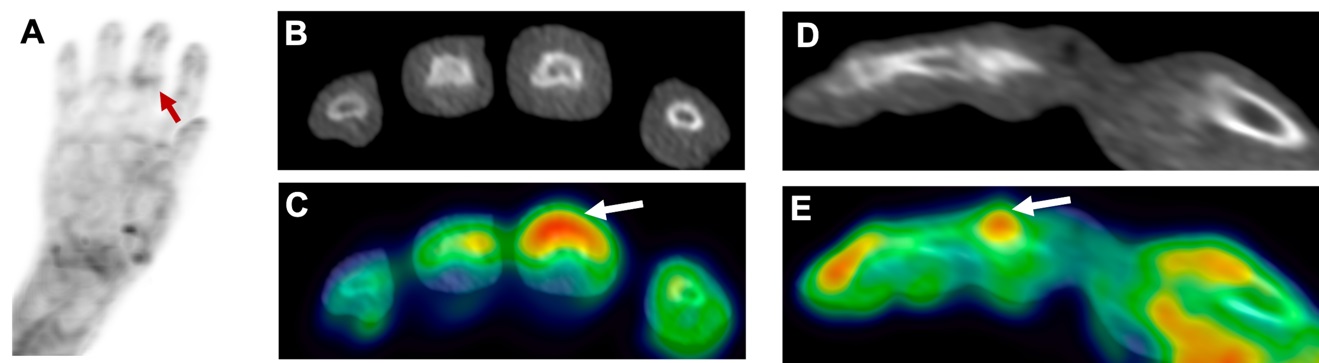 Fig 1: Enthesitis on PET/CT in PsA: Extensor digitorum tendon uptake at the central slip, showing enthesitis; (A) Maximum-intensity projection through the PET scan of the right hand of a participant with PsA showing entheseal uptake at the third PIP joint; axial (B) and sagittal (D) sections through the CT scan of the third PIP joint (grayscale); and axial (C) and sagittal (E) section from the overlay of PET (color) on CT (grayscale).
Fig 1: Enthesitis on PET/CT in PsA: Extensor digitorum tendon uptake at the central slip, showing enthesitis; (A) Maximum-intensity projection through the PET scan of the right hand of a participant with PsA showing entheseal uptake at the third PIP joint; axial (B) and sagittal (D) sections through the CT scan of the third PIP joint (grayscale); and axial (C) and sagittal (E) section from the overlay of PET (color) on CT (grayscale).
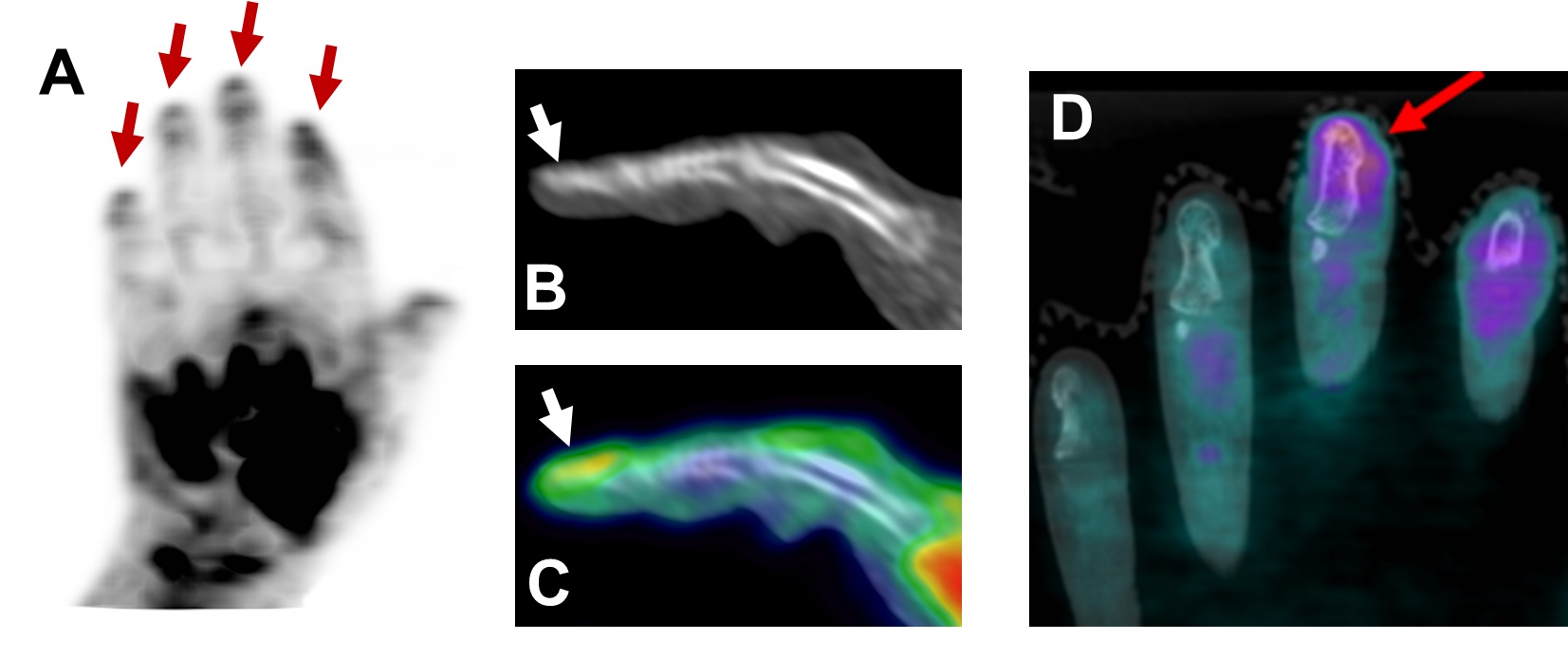 Fig 2: Nail matrix involvement in PsA: (A) Maximum-intensity projection through the PET scan of the left hand of a participant with PsA showing nail involvement; sagittal (B) CT and (C) PET/CT (PET in color, CT in grayscale) of the second digit showing nail bed inflammation. (D) shows nail bed involvement in a participant with PsA from our previous study for comparison.
Fig 2: Nail matrix involvement in PsA: (A) Maximum-intensity projection through the PET scan of the left hand of a participant with PsA showing nail involvement; sagittal (B) CT and (C) PET/CT (PET in color, CT in grayscale) of the second digit showing nail bed inflammation. (D) shows nail bed involvement in a participant with PsA from our previous study for comparison.
To cite this abstract in AMA style:
Raychaudhuri S, Abdelhafez Y, Sarkar S, Raychaudhuri S, Chaudhari A. High-sensitivity 18F-FDG PET/CT: A Diagnostic Tool for Psoriatic Arthritis [abstract]. Arthritis Rheumatol. 2020; 72 (suppl 10). https://acrabstracts.org/abstract/high-sensitivity-18f-fdg-pet-ct-a-diagnostic-tool-for-psoriatic-arthritis/. Accessed .« Back to ACR Convergence 2020
ACR Meeting Abstracts - https://acrabstracts.org/abstract/high-sensitivity-18f-fdg-pet-ct-a-diagnostic-tool-for-psoriatic-arthritis/
