Session Information
Session Type: Abstract Session
Session Time: 2:00PM-3:30PM
Background/Purpose: Cigarette smoking, textile dust, and occupational inhalants all strongly interact with the Human Leukocyte Antigen (HLA) shared epitope for risk of seropositive RA. Recently, we found preceding respiratory tract diseases including asthma, sinusitis, and interstitial lung disease (ILD) are associated with increased risk of RA. In addition, the MUC5B promoter variant was found to increase risk of RA-ILD. Therefore, we aimed (1) to identify gene by respiratory tract disease interactions associated with developing RA and (2) to determine the interaction between MUC5B and respiratory tract diseases for RA risk.
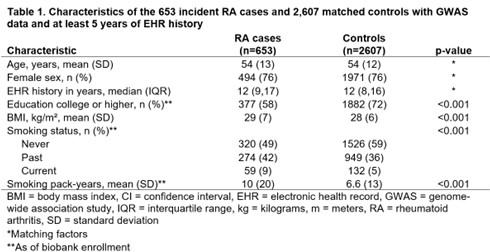
Methods: In this case-control study using a single center biobank, we identified incident RA cases, all confirmed by ACR/EULAR criteria. We matched each RA case to four controls on age, sex, and electronic health record (EHR) duration at index date of RA diagnosis (or assigned date for controls). Genetic exposures included an overall genetic risk score (GRS) including all genetic factors previously associated with RA, an HLA GRS for RA, and the MUC5B promoter variant. We dichotomized the GRSs into “high” and “low” risk by the highest tertile in controls. We obtained preceding respiratory tract diseases from diagnosis codes (positive predictive value 86%). We estimated attributable proportions (AP) and multiplicative odds ratios (OR) with 95% confidence intervals (CI) for RA for each genetic and preceding respiratory disease using conditional logistic regression models, adjusting for age, sex, EHR duration, enrollment year, genetic ancestry by principal components, education, body mass index, and smoking status and pack-years.
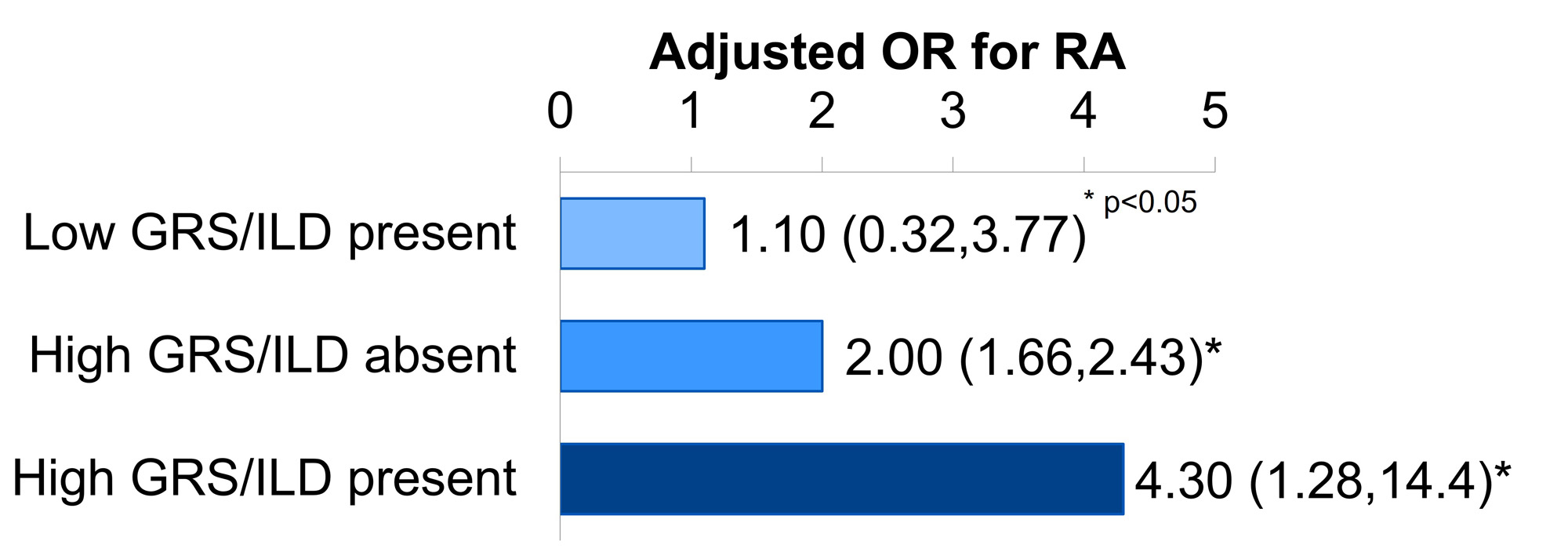
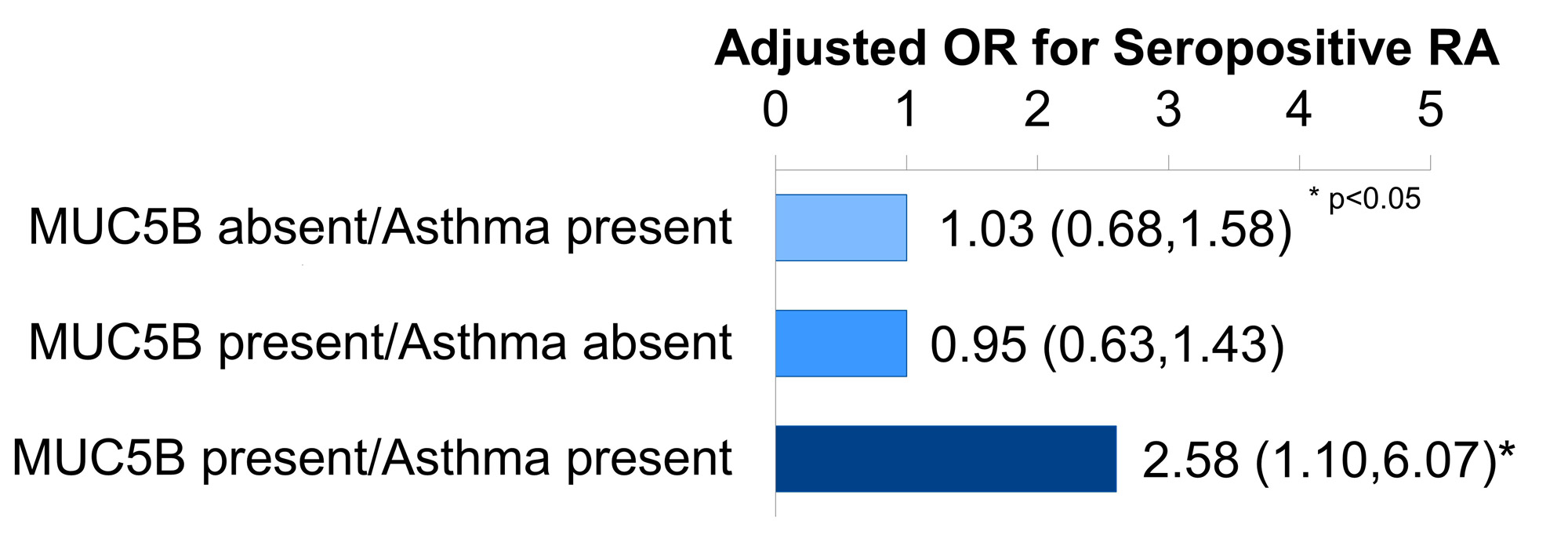
Results: We identified 653 incident RA cases and 2,607 matched controls (mean age 54 years, 76% female, Table 1). The highest tertile of the overall GRS and the HLA GRS were each associated with increased RA risk (OR 2.28, 95% CI 1.89,2.74; OR 2.02, 95% CI 1.67,2.45). ILD and high HLA interacted synergistically for RA risk (OR for both factors 4.30, 95% CI 1.28,14.38 vs. neither; AP 0.51, 95% CI-0.16,1.18; Figure 1). Asthma and the MUC5B promoter variant also interacted synergistically for seropositive RA risk (OR for both factors 2.58, 95% CI 1.10,6.07 vs. neither; AP 0.62, 95% CI 0.24,1.00; Figure 2). Aside from these two synergistic interactions, each GRS exhibited a negative, or “antagonistic,” multiplicative interaction with any respiratory tract disease and sinusitis for RA risk (multiplicative ORs 0.80, 95% CI 0.68,0.94 and 0.73, 95% CI 0.55,0.96, respectively, for the overall GRS).
Conclusion: In summary, ILD in the presence of HLA risk alleles and asthma in the presence of the MUC5B promoter variant were both synergistically associated with developing RA. Future studies should replicate these findings, as they may prove useful for RA screening (i.e. testing for HLA in individuals with ILD) and prevention (i.e. close monitoring for RA in people with asthma who have the MUC5B promoter variant).
To cite this abstract in AMA style:
Kronzer V, Hayashi K, Crowson C, Davis J, McDermott G, Cui J, Losina E, Juge P, Cerhan J, Sparks J. Gene by Respiratory Disease Interactions Associated with Developing Rheumatoid Arthritis [abstract]. Arthritis Rheumatol. 2023; 75 (suppl 9). https://acrabstracts.org/abstract/gene-by-respiratory-disease-interactions-associated-with-developing-rheumatoid-arthritis/. Accessed .« Back to ACR Convergence 2023
ACR Meeting Abstracts - https://acrabstracts.org/abstract/gene-by-respiratory-disease-interactions-associated-with-developing-rheumatoid-arthritis/