Session Information
Date: Tuesday, November 14, 2023
Title: (2095–2140) RA – Diagnosis, Manifestations, and Outcomes Poster III
Session Type: Poster Session C
Session Time: 9:00AM-11:00AM
Background/Purpose: Frailty is established as an important predictor of mortality in the general population.1Rheumatoid arthritis (RA) is associated with higher rates of frailty than the general population,2 yet how frailty impacts important outcomes in RA, such as mortality, is less well understood. We sought to evaluate the relationship between frailty and mortality in a cohort of Veterans with RA.
Methods: Data were obtained from the Veterans Affairs Rheumatoid Arthritis (VARA) Registry from 1/2003 through 12/2021. The VA Frailty Index(VA-FI) is a validated deficit accumulation index based on 31 health deficits mapped from >6000 diagnostic codes found in administrative claims and electronic health records of Veterans. The VA-FI was calculated for each participant at baseline using diagnostic codes with a 3-year look-back period. The VA-FI scores were categorized as robust, pre-frail and frail based on established cutoffs. Death data were obtained from the VA Corporate Data Warehouse vital statistics records. Cox proportional hazard regression models were used to evaluate the relationship between baseline frailty and mortality controlling for baseline age, sex, race, body mass index, anti-cyclic citrullinated peptide (CCP) status, RA disease duration, smoking status, rheumatic disease comorbidity index, use of prednisone, conventional synthetic disease modifying anti-rheumatic drugs (DMARDs) and biologic DMARDs.
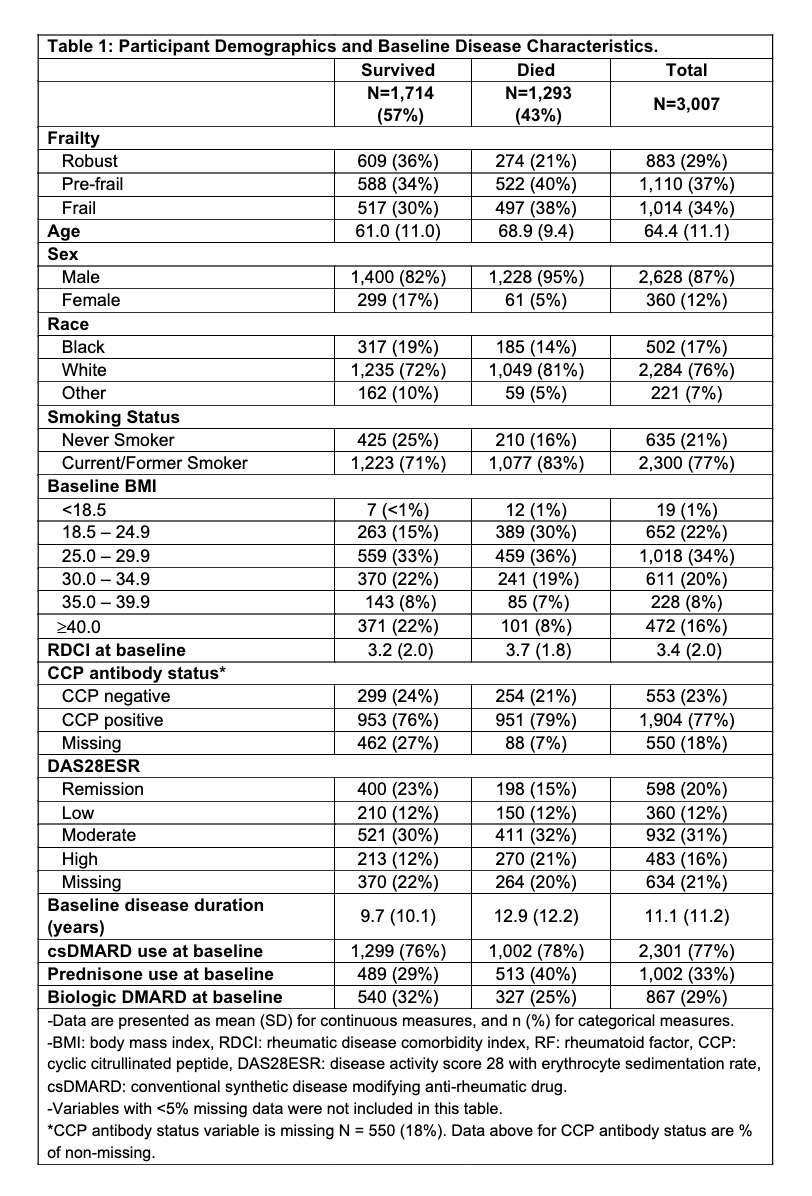
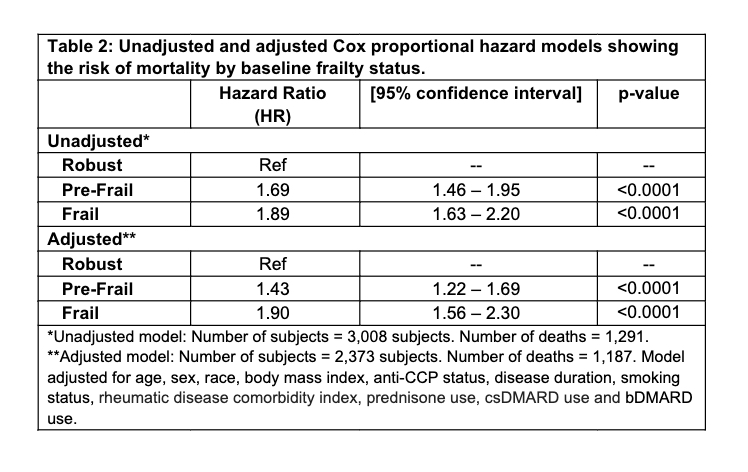
Results: 3,007 Veterans were studied with a mean age of 64.4±11.1 years and 85% were male (Table 1). Over 16,515 person-years of follow-up, 43% (N=1,293) Veterans died. Those who died were older (68.9 vs. 61.0 years), more likely to be male (95% vs. 82%) and had higher rates of high disease activity (21% vs 12%, respectively). Those who died also had higher prevalence of baseline pre-frailty and frailty compared to those who did not die (40% vs. 34% and 38 vs. 30%, respectively). In multivariable models, pre-frailty and frailty were independently associated with a higher risk of death(HR 1.43 [95%CI 1.22-1.69] and 1.90 [95%CI 1.56-2.30], respectively) (Table 2).
Conclusion: Higher baseline frailty is independently associated with an increased risk of death in Veterans with RA. The VA-FI may serve as a tool to aid in early recognition of frailty in people with RA. Further research is necessary regarding the applicability of these findings in informing prognostication and RA disease interventions in vulnerable adults.
References
Orkaby et al. The Burden of Frailty Among U.S. Veterans and Its Association With Mortality, 2002-2012. J Gerontol A Biol Sci Med Sci 2019, 74 (8), 1257–1264.
Gao et al. Frailty in Rheumatoid Arthritis: A Systematic Review and Meta-Analysis. Joint Bone Spine 2022, 89 (4), 105343.
To cite this abstract in AMA style:
Bhide S, Roul P, Singh N, Cannon G, Kunkel G, Mikuls T, England B, Shoback D, Katz P, Garcia J, Orkaby A, Baker J, Wysham K. Frailty Is Associated with Mortality in Veterans with Rheumatoid Arthritis [abstract]. Arthritis Rheumatol. 2023; 75 (suppl 9). https://acrabstracts.org/abstract/frailty-is-associated-with-mortality-in-veterans-with-rheumatoid-arthritis/. Accessed .« Back to ACR Convergence 2023
ACR Meeting Abstracts - https://acrabstracts.org/abstract/frailty-is-associated-with-mortality-in-veterans-with-rheumatoid-arthritis/